Key Points
- A new program called FLOW uses smart data to identify when mental health patients are ready to move back to their family doctors.
- Success depends heavily on “Internal Facilitators,” who act as local champions to bridge the gap between specialty clinics and general medicine.
- Researchers found that high discharge numbers do not always mean a program is working if patients feel forced into the move.
- Shared decision making between providers and patients is the “secret sauce” for a transition that actually sticks.
Discover how a data-driven algorithm and a human touch are reshaping the journey from therapy back to the family doctor.
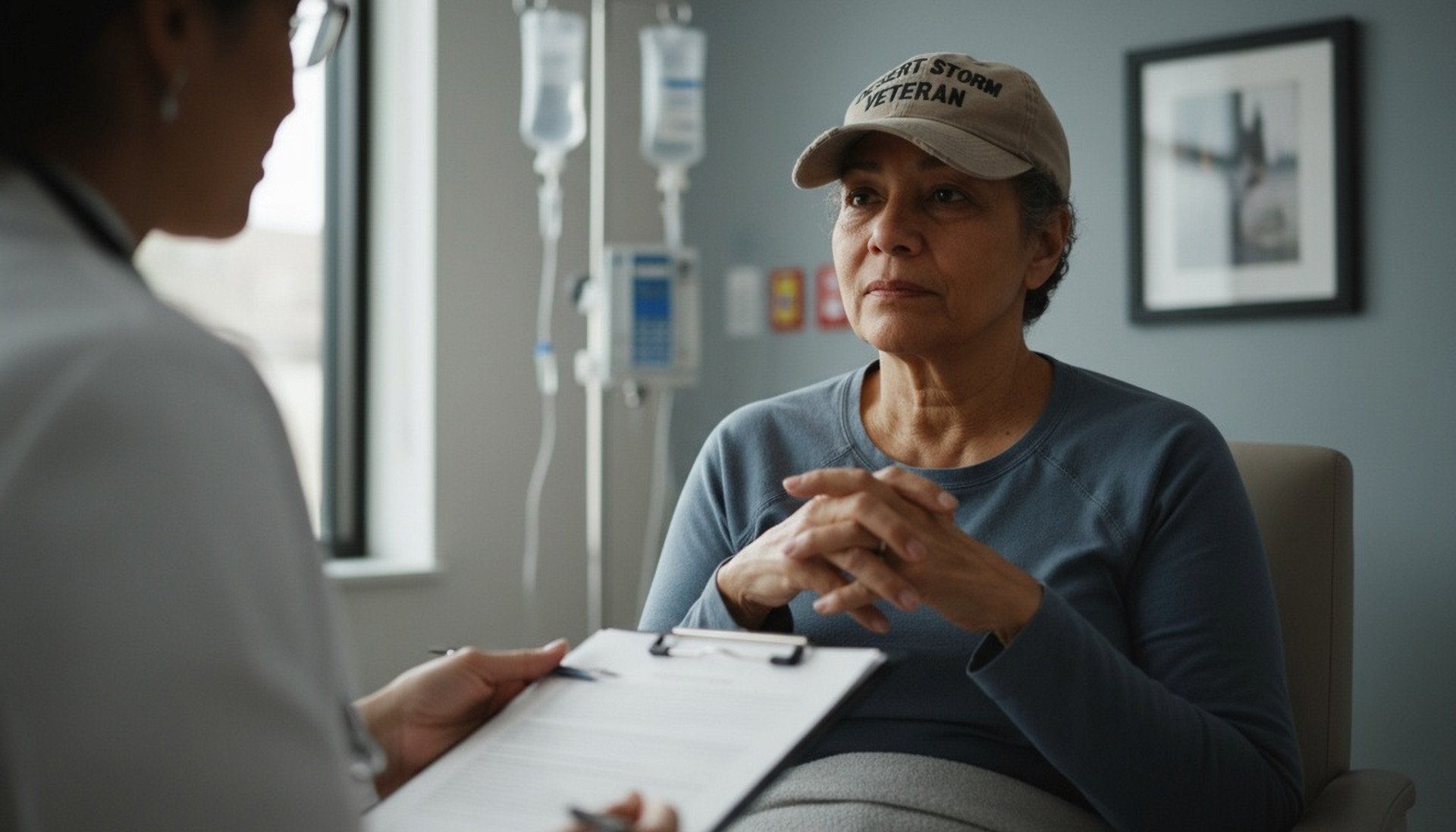
Imagine you have been seeing a specialist for a long-term health goal for months.
One day, you are told your care is moving back to your regular doctor.
For some, this feels like a graduation. For others, it feels like being dropped off a cliff without a safety net.
This delicate handoff is a major hurdle in modern medicine.
When specialty mental health clinics become “clogged” with stable patients, new people in crisis cannot get in.
Scientists recently conducted a deep-dive case study to see how a program called FLOW can fix this.
The Digital Scout for Mental Health
The study focused on an implementation trial within the Veterans Health Administration.
This is the largest integrated health system in the United States. Researchers tracked a program that uses an algorithm to scan electronic medical records.
The algorithm acts like a digital scout.
It looks for patients who have reached a “stabilized” or “recovered” state. These are individuals whose symptoms are managed well enough to be handled by a primary care physician.
The Human Bridge in the Clinic
Data alone cannot move a patient.
The study highlighted the vital role of the Internal Facilitator (IF).
Think of the IF as a local bridge builder who connects two different worlds of medicine.
In successful sites, these facilitators were respected peers who went above and beyond.
They did not just send emails. They sat down with doctors to help them navigate new charting tools.
They turned a cold data list into a warm clinical conversation.
When Numbers Mask the Truth
One of the most surprising findings involved a site that looked like a superstar on paper.
This clinic had the highest number of patient transitions in the entire study. By pure statistics, it was the “top performer”.
However, when the researchers interviewed the patients, the story changed. Many felt they had no choice in the move or were transitioned without their knowledge.
This “success” was actually a struggle because the patients felt abandoned rather than supported.
The Power of the Shared Choice
The research proves that shared decision making is not just a polite suggestion.
It is a functional requirement for long-term health. Patients need to feel like they are “graduating” with their doctor’s blessing.
When a patient agrees to the move, they are more likely to stay engaged with their care.
If they feel coerced, they might stop taking medication or end up back in the emergency room. True success is a mix of high-tech data and high-touch empathy.
Why it Matters
For the general public, this study offers a glimpse into the future of “stepped care.”
It suggests that your medical record might soon help your doctor know exactly when you are ready for the next phase of recovery.
This approach ensures that specialized resources are available for those who need them most.
It also empowers stable patients to manage their health within their familiar primary care setting. It turns the “revolving door” of mental health care into a clear, upward path.
Smith, T. L., Yusuf, Z. I., Kim, B., Amspoker, A. B., & Hundt, N. E. (2026). An external facilitation case study analysis of an implementation trial of FLOW: A program for improving the transition of patients with mental health disorders back to primary care. Psychological Services, 23(1), 91–100. https://doi.org/10.1037/ser0000898

