Avoidant personality disorder and social anxiety disorder are both conditions marked by fear of judgment and avoidance of social situations, but they differ in scope and severity.
Social anxiety disorder is typically situation-specific, such as fear of public speaking, while avoidant personality disorder involves a pervasive pattern of low self-esteem, hypersensitivity to criticism, and avoidance across nearly all areas of life.
Understanding the differences is crucial for accurate diagnosis and effective treatment.

This article is for informational and educational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health provider with any questions you may have regarding a medical or mental health condition. Never disregard professional advice or delay in seeking it because of something you have read on this site.
Key Takeaways
- Shared traits: Both AVPD and SAD involve fear of judgment and social avoidance.
- Scope: SAD is situation-specific; AVPD affects nearly all social areas.
- Self-view: AVPD comes with deep feelings of inferiority; SAD allows healthier self-esteem.
- Life impact: AVPD causes broad difficulties, while SAD mainly disrupts specific situations.
- Treatment: SAD often responds well to CBT and medication; AVPD needs longer-term therapy.
What Is Social Anxiety Disorder (SAD)?
Social Anxiety Disorder (SAD)—also known as social phobia—is an anxiety condition marked by intense fear of scrutiny or negative judgment in everyday social and performance situations.
Unlike ordinary shyness, this fear is persistent (lasting at least six months), often avoids daily life, and significantly impairs functioning at work, school, or in relationships.
Symptoms and triggers
Common physical symptoms include blushing, sweating, trembling, rapid heartbeat, nausea, dizziness, or a mind that “goes blank,” especially during social interaction or performance tasks.
Triggers range from speaking in public, meeting new people, to everyday actions like eating in front of others or using public restrooms (National Institute of Mental Health).
Causes and risk factors
SAD likely results from a mix of genetic predisposition (family history), neurochemical imbalances, and environmental influences such as childhood teasing, bullying, overprotective parenting, or traumatic social events (National Institute of Mental Health).
How SAD is diagnosed
Diagnosis typically relies on DSM‑5 criteria: enduring fear or anxiety in social situations, avoidance or distress, lasting six months or more, and significantly affecting daily functioning—while excluding other medical or mental health causes.
Common treatment approaches
First-line treatments include Cognitive Behavioral Therapy (CBT)—especially exposure-based strategies—and, when needed, medications like SSRIs, SNRIs, beta-blockers, or benzodiazepines.
Many people improve markedly when therapy is combined with medication.
What Is Avoidant Personality Disorder (AVPD)?
Avoidant Personality Disorder (AVPD) is a Cluster C personality disorder marked by a long-standing pattern of social inhibition, hypersensitivity to criticism, and intense feelings of inadequacy and inferiority—despite a deep desire for connection (National Library of Medicine).
Core traits and symptoms
- Persistent avoidance of social relationships unless certain of acceptance
- Preoccupation with fear of rejection or humiliation
- Self-view as socially inept, personally unappealing, or inferior
- Reluctance to try new things due to embarrassment or shame
Causes and risk factors
AVPD likely arises from a mix of genetic predispositions (e.g., behavioral inhibition), early temperament, and adverse childhood experiences such as rejection, emotional neglect, or a “fearful” attachment style (National Library of Medicine).
How AVPD is diagnosed
Diagnosis typically occurs in adulthood, based on enduring, inflexible behavior patterns that meet DSM‑5 criteria—requiring at least four of seven specific symptoms such as social inhibition, fear of criticism, or views of self as inferior.
Clinicians also rule out other mental health conditions.
Treatment challenges and approaches
Treating AVPD is challenging due to entrenched avoidance and trust barriers.
Talk therapies—like CBT, psychodynamic therapy, schema therapy, interpersonal therapy, and social skills training—are the main approaches.
Medications aren’t approved for AVPD itself, according to the National Library of Medicine, though they may help manage comorbid anxiety or depression.
Similarities Between AVPD and SAD
Shared symptoms and behaviors
Both Avoidant Personality Disorder (AVPD) and Social Anxiety Disorder (SAD) involve an intense fear of negative evaluation, including criticism, rejection, or embarrassment, which leads to social avoidance or extreme discomfort in social situations.
Both conditions can significantly disrupt daily functioning, affecting relationships, work, and social life.
Why are they often confused?
These disorders are frequently mistaken for each other because of their overlapping symptoms—like avoidance and low self-confidence—as well as their shared root in social fear.
AVPD is often seen as a more pervasive condition, while SAD is situational, which further blurs distinctions in everyday discussions.
Can someone have both?
Yes. According to research, there’s a moderate co-occurrence rate found between the two disorders.
Key Differences Between AVPD and SAD
Below are some of the key differences between avoidant personality disorder and social anxiety disorder:
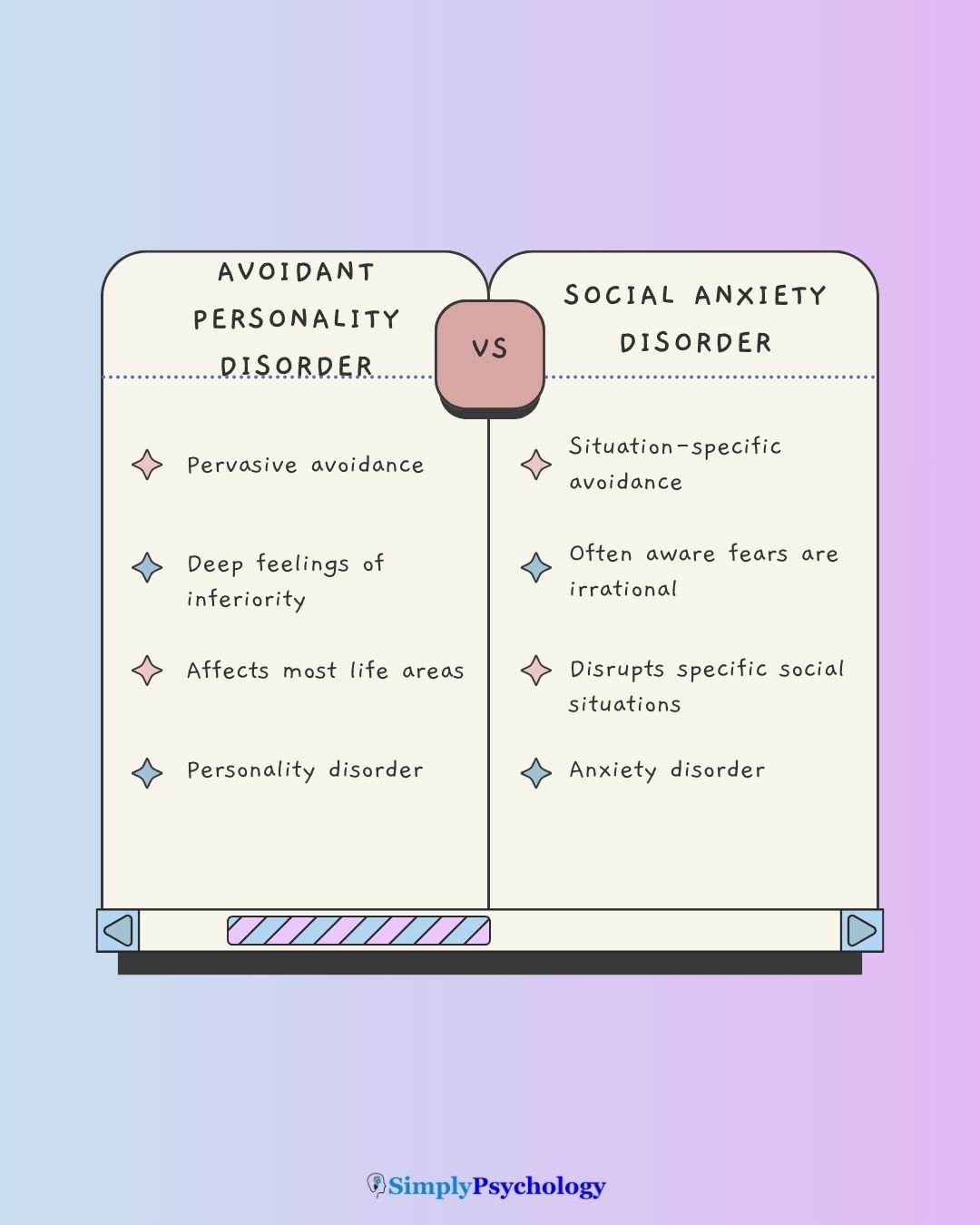
Scope of avoidance
- AVPD involves avoiding nearly all social interactions due to pervasive feelings of inadequacy and rejection.
- SAD tends to involve avoidance only in specific socially stressful situations, such as public speaking or meeting new people.
Differences in causes and triggers
- Both conditions are thought to be linked to negative childhood experiences, but AVPD is more strongly associated with emotional neglect and pervasive self-esteem issues.
- SAD is often triggered by performance anxiety—fear of embarrassment or negative evaluation in specific social contexts.
Self-esteem and self-perception
- People with AVPD internalize feelings of inferiority and believe others judge them harshly based on that view.
- In SAD, individuals usually understand their fears are irrational and maintain healthier self-esteem.
Impact on daily functioning
- AVPD leads to broad impairment across relationships, work, and daily life.
- SAD impacts functioning primarily in anxiety-provoking situations, while other areas may remain relatively unaffected.
Treatment differences
- SAD is well-researched and typically responds well to CBT, exposure therapy, and medications (SSRIs, beta-blockers).
- AVPD treatment focuses on deeper self-concept issues using schema, psychodynamic, or group therapy. Medication is not a recommended treatment for personality disorders, but it may be used for co-occurring symptoms of anxiety.
Comparison table
| Feature | AVPD | SAD |
|---|---|---|
| Scope of avoidance | Broad, pervasive across social life | Specific to particular social situations |
| Causes & triggers | Emotional neglect; deep-seated self-criticism | Performance/social evaluation anxiety |
| Self-esteem & self-perception | Poor self-image; believes negative self-view is justified | Aware fears are irrational; preserves self-esteem |
| Impact on functioning | Widespread impairment in relationships, work, daily life | Functioning often intact outside anxiety-triggering situations |
| Treatment differences | Therapy focusing on self-concept (schema, group); meds for comorbidity | CBT, exposure techniques, meds like SSRIs or beta-blockers |
| Relation between disorders | Related but distinct—AVPD rooted in identity; not just severe SAD | Often comorbid, but conceptually separate |
Is AVPD just a severe form of social anxiety?
Not exactly. While Avoidant Personality Disorder (AVPD) and Social Anxiety Disorder (SAD) overlap in social avoidance and fear of criticism, they are distinct diagnoses.
Individuals with SAD typically recognise their fears as exaggerated, while people with AVPD genuinely view themselves as inferior and unworthy of connection.
Some experts consider AVPD to be on the extreme end of a continuum with SAD. Yet, substantial evidence supports the idea that they’re not just differing in severity, but also in underlying self-perception and avoidance patterns.
Daily Life Impact and Coping Strategies
Living with social anxiety disorder (SAD) or avoidant personality disorder (AVPD) can shape almost every aspect of daily life—from relationships to school or work performance. While the conditions overlap in avoidance, the depth of emotional impact often differs.
Relationships and social life
Both SAD and AVPD can make forming and maintaining relationships difficult. People with SAD often describe losing friendships or romantic opportunities due to fear of judgment. As one Redditor admitted:
“I’ve lost jobs cos of it, lost friends cos of it and am too afraid to speak to women…”
For those with AVPD, the struggle runs even deeper, tied to core feelings of inadequacy. One person explained:
“Social anxiety feels more like irrational panic… Whereas AVPD feels a lot more specific, and ingrained. … I don’t want people to see who I really am and how worthless, burdensome or disappointing the real me is.”
Work and school functioning
SAD can undermine focus and performance, especially in academic or professional environments:
“From my experience… I was so anxious the whole time I couldn’t even concentrate after uni…”
Meanwhile, AVPD may prevent individuals from even attempting certain paths, leading to long-term isolation. As one person described:
“I get tight shoulders and anxiety passing people in public. I overthink. I dread human interaction. I am 31 and never been in a relationship.”
Coping strategies and peer support
Despite these challenges, many find gradual progress through small steps and community support. One person who overcame SAD emphasized:
“The key is not to hide yourself in the comfort of solitude. Once the social exposure becomes habitual the anxiety begins to slowly subside.”
Similarly, those with AVPD note that practice—even when uncomfortable—can make interactions feel less overwhelming:
“I still avoid social interactions. But you have to force yourself and put yourself out there. Try to talk about everyday things and joke about it. I’m still working on this but it’s definitely improving. Using humor with things and not taking things seriously works wonders with socializing.”
These reflections highlight both the barriers and the possibilities—showing that while the road is challenging, even small social steps can create meaningful change.
When to seek professional support
Signs to Look For
It may be time to reach out if anxiety or avoidance starts disrupting your life—this includes skipping work or school, avoiding social interactions, or struggling to maintain relationships because of fear or self-doubt.
If social anxiety or avoidance persists for six months or longer and significantly impacts multiple areas (work, school, relationships), that’s a strong indicator that professional support could help.
For AVPD, early intervention is key: seeking help as soon as symptoms appear can reduce long-term disruptions in your life and relationships.
Remember…
Seeking help doesn’t mean you’re weak—it’s a proactive step toward living more fully. You don’t have to wait until things fall apart.
Talking to a GP, therapist, or counselor can lead to strategies that build confidence and reduce avoidance.
Even if you’re not sure whether your experiences “qualify,” starting a conversation can bring clarity—and pathway toward more manageable, meaningful connections.
Resources
National Institute of Mental Health: Social Anxiety Disorder: What You Need to Know
National Library of Medicine: Avoidant Personality Disorder
References
Hummelen, B., Wilberg, T., Pedersen, G., & Karterud, S. (2007). The relationship between avoidant personality disorder and social phobia. Comprehensive psychiatry, 48(4), 348-356.
Lampe, L., & Malhi, G. S. (2018). Avoidant personality disorder: current insights. Psychology research and behavior management.
Taylor, C. T., Laposa, J. M., & Alden, L. E. (2004). Is avoidant personality disorder more than just social avoidance? Journal of personality disorders, 18(6), 571-594.
Torvik, F. A., Welander-Vatn, A., Ystrom, E., Knudsen, G. P., Czajkowski, N., Kendler, K. S., & Reichborn-Kjennerud, T. (2015). Longitudinal associations between social anxiety disorder and avoidant personality disorder: A twin study. Journal of Abnormal Psychology, 125(1), 114. https://doi.org/10.1037/abn0000124
Weinbrecht, A., Schulze, L., Boettcher, J., & Renneberg, B. (2016). Avoidant personality disorder: a current review. Current psychiatry reports, 18(3), 1-8.



