If you feel like every other person on your social media feed suddenly has an ADHD diagnosis, you aren’t imagining things.
The rates of diagnosis—especially among adults—have surged in recent years, leading many to wonder: Is ADHD becoming a trend, or are we just finally paying attention?

It is easy to dismiss this rise as the result of viral videos or a “medicalized society.” However, according to Dr. Russell Barkley, a clinical psychologist and one of the world’s leading researchers on ADHD, the data tells a much more complex story.
The reality isn’t that we are creating new cases out of thin air; it’s that we are finally identifying a “Lost Generation” of people who have been struggling in silence for decades.
This article cuts through the noise to explain exactly why the numbers are up, drawing on insights from Dr. Barkley, Dr. Megan Anna Neff, and ADHD expert Caren Magill.
The “Trend” Myth: Are We Really Overdiagnosed?
The short answer from the experts is: No, not broadly.
Dr. Russell Barkley argues against the idea of widespread overdiagnosis. He suggests that current diagnosis rates are simply catching up to the actual number of people living with ADHD.
Dr. Barkley points to the hard numbers to validate this:
- Prevalence vs. Prescriptions: In the US, approximately 6.6% of adults are on ADHD medication.
- Actual Cases: This aligns closely with the estimated adult prevalence of 5–6%.
If ADHD were truly being overdiagnosed on a massive scale, we would expect prescription rates to vastly outpace the estimated prevalence. Instead, they match.
Key Insight: Dr. Barkley suggests we view this rise not as a “flood” of new cases, but as turning on the lights in a previously dim room. The people were always there; we just couldn’t see them before.
Why Now? The “Perfect Storm” for Diagnosis
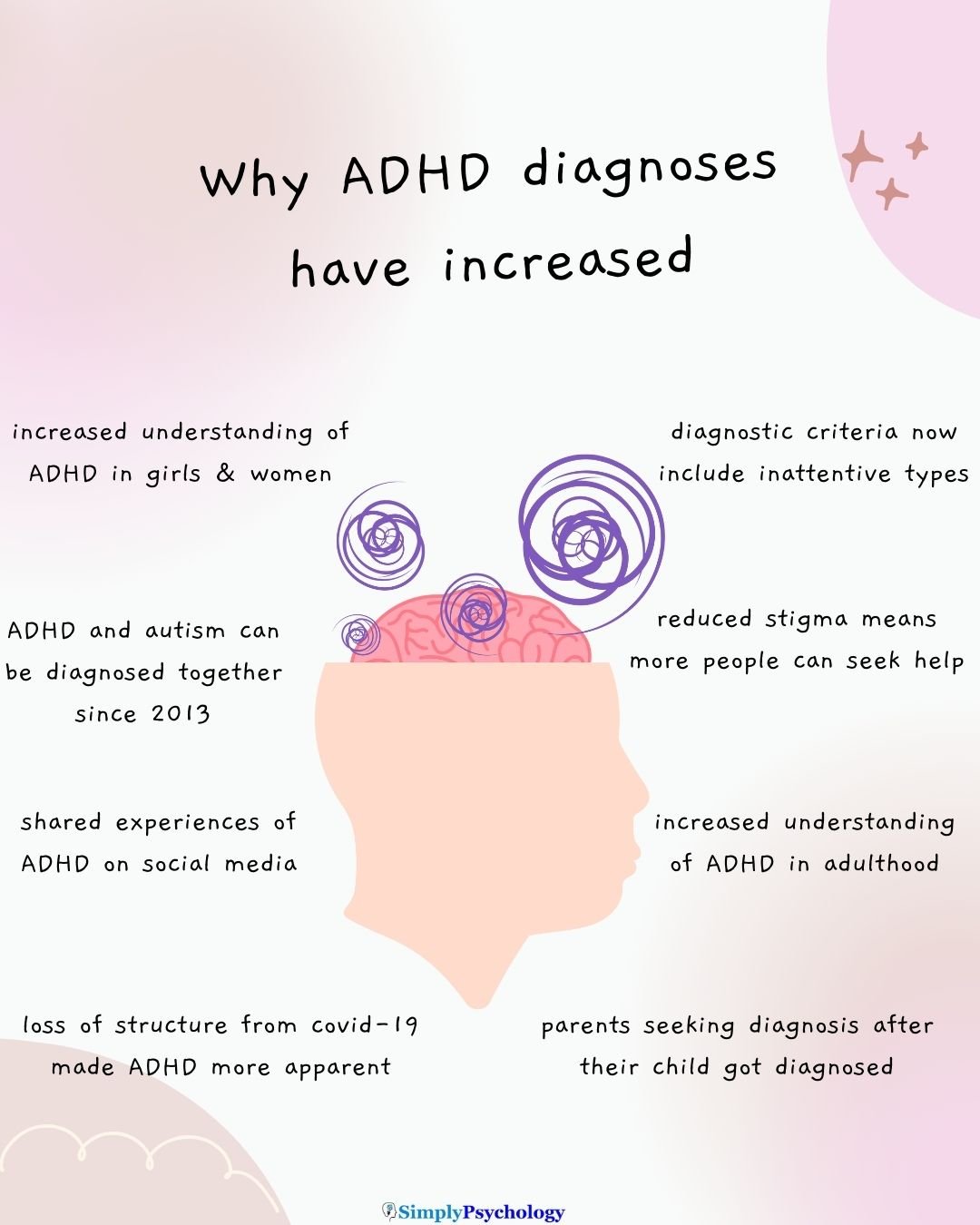
If these people were always there, why are they all getting diagnosed now? Caren Magill, an ADHD expert and author, explains that the surge is due to a collapse of coping mechanisms, particularly since 2020.
Magill notes that the rate of adult diagnosis has more than doubled since 2020. She attributes this to three specific triggers:
- The Loss of Structure: When the pandemic hit, the external routines (office hours, commutes, gym classes) that held people’s lives together vanished. Without this “scaffolding,” the internal chaos of ADHD became impossible to ignore.
- The “Child-to-Parent” Pipeline: Magill highlights that ADHD is highly hereditary, with up to a 70% chance of passing it to children. Many adults only realize they have it when sitting in a doctor’s office getting their child diagnosed.
- The Collapse of Masking: Those labelled as “high-functioning” adults often use “compensatory methods”—like extreme anxiety or perfectionism—to hide their symptoms. When the stress of the world increased (i.e. the COVID-19 pandemic), these masks fell apart.
The “Lost Generation”: Women and Inattentive Types
For decades, the medical standard for ADHD was a hyperactive 12-year-old boy. If you didn’t fit that mold, you were likely missed.
Dr. Megan Anna Neff, a clinical psychologist, describes a “Lost Generation” of women, genderqueer people, and people of color who were overlooked because they didn’t act out in class.
The Criteria Changed
Dr. Barkley explains that a massive shift occurred when diagnostic manuals (the DSM-4 and DSM-5) finally recognized the “Inattentive Presentation.”
- Previously, you had to be hyperactive to get help.
- When “inattentive” criteria were added, the prevalence of the disorder in US children jumped from about 2–5% to 5–8%.
This wasn’t an inflation of the disease; it was the inclusion of the quiet daydreamers who had been suffering without support.
ADHD and co-existing Autism
Prior to the release of the DSM-5 in 2013, ADHD could not be diagnosed if someone already had a diagnosis of autism.
If a clinician diagnosed a child with autism (or Pervasive Developmental Disorder), they were instructed not to diagnose ADHD, even if the child displayed clear symptoms of hyperactivity or inattention.
Why this matters: because of this rule, many autistic individuals have missed out on support for co-existing ADHD, which we now know commonly co-exists together (with many people described as being AuDHD).
This can also explain why there is an increase in ADHD diagnoses since 2013 – because many autistic people are now able to receive a diagnosis of ADHD when this was not an option for them previously.
Where Overdiagnosis (and Underdiagnosis) Actually Happens
While the experts generally agree that broad overdiagnosis is a myth, they acknowledge that misdiagnosis does happen. It is critical to look at the specific statistics to understand where the errors lie.
Potential Overdiagnosis Areas
There are specific pockets where numbers may be inflated:
- College Campuses: Dr. Barkley notes that students may feign symptoms to get stimulants for studying.
- Regional Spikes: In Stockholm, Sweden, diagnosis rates for adolescent males are estimated to reach 15%, far above the global expected average of 5–7%. This suggests that in some highly medicalized areas, the bar for diagnosis may be too low.
The Reality of Underdiagnosis
Conversely, huge groups are still being left behind. Dr. Neff and recent studies point to significant racial disparities:
- Racial Gaps: Research indicates that non-Hispanic Black and Hispanic children have significantly lower odds of receiving an ADHD diagnosis compared to non-Hispanic White children, despite exhibiting similar symptoms.
- The Consequence: These children often face disciplinary action in school for behavior that would trigger a medical referral for their White peers.
Conclusion: It’s About Visibility, Not Virality
The rise in ADHD diagnoses can feel overwhelming, but the experts agree it is largely a positive correction of historical neglect. As Dr. Neff argues, identifying people who “have always been here” allows them to access the support they were previously denied.
Whether it is a woman realizing her “laziness” is actually executive dysfunction, or a parent recognizing their own struggles in their child, the data suggests we aren’t overdiagnosing—we are finally just listening.
Next Steps: What to Do If You Resonate With This
If you suspect you might be part of the “Lost Generation,” here are three concrete steps to take:
- Look for “Life Evidence”: Before your appointment, write down examples of symptoms from childhood. ADHD is a lifelong condition; a diagnosis requires proof that symptoms existed before age 12.
- Check for “Lookalikes”: Burnout, anxiety, and trauma can mimic ADHD. Dr. Barkley recommends a thorough evaluation to rule these out.
- Seek Neuroaffirming Care: If possible, find a clinician who understands “inattentive” or “high-masking” presentations to avoid being dismissed because you “have a job” or “did well in school.”

