Mindfulness-based cognitive therapy (MBCT) combines elements of mindfulness practice and cognitive behavioral therapy to help individuals develop greater awareness and acceptance of their thoughts, emotions, and experiences in order to cultivate resilience and prevent relapse in depression and anxiety.
This psychotherapy was designed to help people who experience repeated episodes of depression and to help prevent depression from returning.
MBCT usually takes the form of 8 weekly sessions, with guided meditations accompanying the program so that participants can practice skills at home throughout the course.

This article is for informational and educational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health provider with any questions you may have regarding a medical or mental health condition. Never disregard professional advice or delay in seeking it because of something you have read on this site.
What is Mindfulness?
Jon Kabat-Zinn, one of the founders of mindfulness-based therapies defines mindfulness as:
“Awareness that arises through paying attention, on purpose, in the present moment, non‑judgmentally… in the service of self‑understanding and wisdom.”
Mindfulness has grown in popularity over recent years and can involve breathing methods, guided imagery, and other practices to relax the body and mind and help reduce stress and anxiety.
Goals of mindfulness-based cognitive therapy
The MBCT website outlines three ways in which mindfulness practice can help people:
- To help you understand what depression is.
- To help you discover what makes you vulnerable to downward mood spirals and why you get stuck at the bottom of the spiral.
- To help you see the connection between negative thinking and downward spirals. This includes setting unrealistically high standards for yourself, feelings that you are simply not good enough, and ways you may lose touch with what makes life worth living.
Psychologist Dr Francia Day explains that:
“Mindfulness-based cognitive therapy teaches that thoughts are not necessarily facts and noticing them, rather than reacting to them, can help shift your experience… It can help people feel empowered rather than victims of their experience.”
MBCT vs. CBT
MBCT and cognitive behavioral therapy (CBT) help recognize unhelpful thoughts and involve learning that these thoughts aren’t facts but something one can take a wider view of.
They both aim to make the person feel less likely to be drawn into automatic reactions to thoughts, feelings, and events. Also, both CBT and MBCT are short to medium-term therapies, and both tend to work best for those with depression and anxiety.
The main difference between the two therapies is that MBCT uses mindfulness, which involves recognizing what is going on in the present moment, and how an individual is thinking, feeling, and experiencing in the present moment.
CBT, on the other hand, uses cognition to understand negative thought processes – it is very analytical, with clients charting their emotions and reactions as homework.
So, while MBCT encourages noticing what is going on around the person, CBT encourages the person to constantly notice their thoughts.
CBT also encourages the individual to push out unhelpful thoughts, whereas MBCT involves letting negative thoughts drift through the mind without judgment.
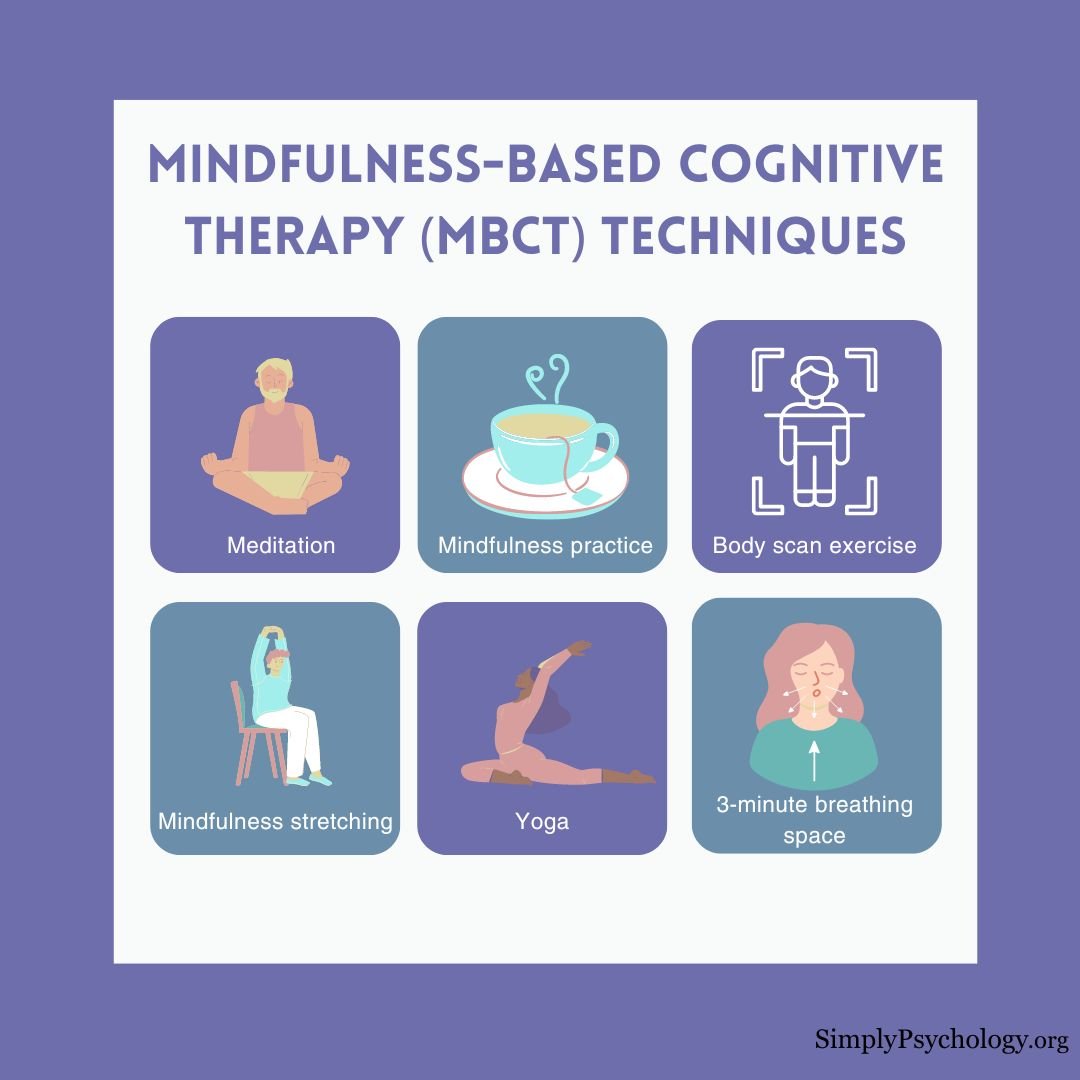
Techniques
MBCT uses a combination of mindfulness meditation, cognitive restructuring, and psychoeducation to help individuals recognize and modify unhelpful thought patterns, increase self-compassion, and develop a more present-focused and accepting mindset.

Below are some of the techniques specifically used in MBCT:
Meditation
People may learn meditative techniques during MBCT. This can involve practicing guided or self-directed meditation that helps them gain a greater awareness of their body, thoughts, and breathing.
Body scan exercise
This exercise typically involves lying down in a comfortable position and focusing on the breath, noticing the rhythm and sensation of this.
Then, the individual will be asked to bring awareness to different areas of their body, usually beginning at the toes and moving up through the body until they reach the top of the head.
During this awareness, they will be asked to note how each part of their body feels, the texture of clothing against their skin, any temperature or sensations they feel, and whether areas feel sore or heavy/light.
Mindfulness practices
This involves becoming more aware of the present moment. It is something that can be practiced during meditation but can also be incorporated into the everyday activities people complete.
For instance, mindfully making a cup of tea, mindfully washing up, and mindful cooking.
Mindfulness stretching
This technique involves stretching the body in a mindful way to help bring awareness to the body and the mind.
Rushing straight into exercise can be a missed opportunity to prepare the mind and body for physical exertion.
Mindfulness stretching can also add more benefits to exercise, such as increased awareness and a sense of balance.
Yoga
MBCT may also encourage people to practice yoga poses that can help facilitate mindful stretching of the body.
Some poses can help to open up the chest or other areas of the body, bring awareness to parts of the body, and incorporate working and moving with the breaths.
3-minute breathing space
People in MBCT may be taught what is known as the 3-minute breathing space technique. This focuses on three steps, each one minute in duration:
- Observing the experience (the individual brings awareness to how they are doing at that moment).
- Focusing on the breath.
- Attending to the body and any physical sensations that might be experienced.
These techniques of MBCT allow the individual to move away from automatic and unhelpful responses, towards an understanding that there are other ways to respond to situations.
By developing a mindfulness meditation routine, individuals can use the techniques whenever they start to feel overwhelmed by negative emotions.
The idea is that when sadness occurs and starts to bring up all the usual negative associations that trigger depressed feelings, the individual is equipped with the tools that will help them substitute negative thought patterns with positive ones.
What Can Mindfulness-Based Cognitive Therapy Help With? (And How It May Help)
Dr. Zindel Segal, one of MBCT’s founders expresses that:
“MBCT has its strongest evidence base associated with preventing depressive relapse or treating residual depressive symptoms.”
Over time, it has been explored as a supportive approach for a range of mental health conditions that involve patterns of negative thinking, emotional distress, or difficulty with regulation.
Areas Where MBCT May Be Helpful
MBCT was specifically designed to address the cyclical nature of depression, but it has also been applied in contexts such as:
- Generalized anxiety disorder (GAD) and other anxiety-related difficulties
- Obsessive-compulsive disorder (OCD)
- Addictions and substance use challenges
- Bipolar disorder
- Psychotic disorders
- Low mood and chronic stress
- Depression linked to chronic illness or brain injury (e.g., TBI)
- Treatment-resistant depression
While MBCT is not intended to replace clinical care, it may be used alongside other treatments to support emotional awareness and coping. As with any psychological approach, its suitability can depend on individual needs and circumstances.

How MBCT May Support Mental Health
MBCT is not focused on eliminating difficult thoughts or emotions but instead offers tools to change the way individuals relate to their internal experiences.
The following benefits have been reported in research studies and clinical settings:
Responding to Negative Thinking
MBCT helps people recognize patterns such as rumination, tunnel vision, or automatic negative thoughts (ANTs).
Rather than trying to suppress these thoughts, mindfulness practices encourage a gentle awareness of them as mental events—not facts—that tend to come and go.
Mindfulness interventions have shown promise for improving OCD symptoms (Pseftogianni et al., 2023).
Supporting Recovery and Reducing Relapse
In a UK-based evaluation of MBCT across five mental health services, 96% of participants sustained their recovery during the treatment period. The study also found a significant reduction in residual symptoms that are often linked to relapse (Tickell et al., 2019).
A separate trial comparing MBCT with antidepressant treatment found that 52% of participants in the MBCT group did not relapse, compared to 48% in the medication group. Researchers suggested that MBCT may be similarly effective in preventing depressive relapse (Kuyken et al., 2015).
Strengthening Emotional Awareness and Regulation
Through techniques like body scans, mindful breathing, and the 3-minute breathing space, MBCT offers practical ways to become more aware of emotional shifts as they happen. This can help reduce the likelihood of being overwhelmed by intense emotions or caught in reactive patterns.
Fostering Self-Compassion
Many mindfulness-based exercises used in MBCT emphasize kindness and acceptance toward oneself. This includes developing a more balanced inner dialogue—especially during moments of sadness, frustration, or shame.
Building Everyday Coping Skills
The skills taught in MBCT can often be applied to daily life. These include grounding techniques, breathing exercises, and mindful movement practices like yoga or stretching.
With regular practice, individuals may find they are better equipped to handle moments of stress, uncertainty, or emotional discomfort.
Considerations
MBCT has potential limitations to consider. It may not be suitable for severe mental health conditions, and consistent commitment to mindfulness practice is necessary for its effectiveness.
Therapist training and competence are crucial for delivering MBCT successfully. Inadequate training or experience in mindfulness-based approaches can impact the quality of therapy and outcomes for individuals.
While MBCT has shown effectiveness in reducing relapse rates for depression and anxiety, it may not provide foolproof protection against future relapses. Some individuals may still experience relapses despite engaging in MBCT.
Further research is needed to explore its long-term effects, compare it to other treatments, and determine its efficacy for specific populations and conditions.
These limitations highlight the importance of considering individual suitability and seeking professional guidance when using MBCT.
Please discuss MBCT with a trained healthcare professional for more information.
How Was MBCT Developed?
Mindfulness-Based Cognitive Therapy (MBCT) emerged in the 1990s when psychologists Jon Teasdale and Phillip Barnard identified two modes of mind: the goal-driven “doing” mode and the accepting “being” mode. While traditional therapy emphasized thinking, lasting emotional change was linked to the being mode—central to mindfulness.
Building on this insight, Zindel Segal, Mark Williams, and Jon Kabat-Zinn combined mindfulness practices with cognitive therapy, creating MBCT as a program specifically designed to help people with recurrent depression recognize and step out of negative thought spirals before they escalate.
How to get the most out of mindfulness based cognitive therapy
How can I seek MBCT?
It’s important to talk to your doctor about your symptoms to determine if this is the right approach for you. Talk to your doctor or consider searching an online therapist directory to find an MBCT therapist.
Depending on the availability of trained MBCT therapists in your area, finding classes may be challenging. An MBCT therapist is a mental health professional who has additional training in mindfulness-based practices and techniques and is skilled in teaching these techniques to others.
Mindfulness has become increasingly popular for promoting mental health, so even mental health professionals who are not specifically trained in MBCT may incorporate some aspects of mindfulness practices in their therapy sessions.
It may be worth contacting therapists and asking if this is something they offer in their treatment.
What can I expect from MBCT sessions?
MBCT is a group intervention that lasts for eight weeks. Each session lasts for about 2 hours, and there is usually a one-day-long class, typically after the 5th week.
Much of the work done in MBCT is completed outside of the sessions. Participants are asked to do homework, which includes listening to recorded guided meditations and trying to cultivate mindfulness in their daily lives.
These homework assignments are usually 45 minutes long, six days a week.
Things to consider before starting MBCT
Much of the research on MBCT is still ongoing as it is a relatively new practice; therefore, the long-term effects are not as well known yet.
MBCT involves a lot of commitment, so you need to be prepared to attend the weekly sessions and complete the homework assignments to ensure you get the most out of the therapy.
In addition to checking credentials, it’s important to find an MBCT therapist who you feel comfortable with.
Further Information
- Sipe, W. E., & Eisendrath, S. J. (2012). Mindfulness-based cognitive therapy: theory and practice. The Canadian Journal of Psychiatry, 57(2), 63-69.
- MacKenzie, M. B., & Kocovski, N. L. (2016). Mindfulness-based cognitive therapy for depression: trends and developments. Psychology research and behavior management.
References
Bank, S., Burgess, M., Sng, A., Summers, M., Campbell, B., & McEvoy, P. (2020). Stepping Out of Social Anxiety. Perth, Western Australia: Centre for Clinical Interventions.
Kim, Y. W., Lee, S. H., Choi, T. K., Suh, S. Y., Kim, B., Kim, C. M., Cho, S. J., Kim, J. M., Yook, K., Ryu, M., Song, S. K. & Yook, K. H. (2009). Effectiveness of mindfulness‐based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depression and anxiety, 26(7), 601-606.
Kuyken, W., Hayes, R., Barrett, B., Byng, R., Dalgleish, T., Kessler, D., Lewis, G., Watkins, E., Brejcha, C., Cardy, J., Causley, A., Cowderoy, S., Evans, A., Gradinger, F., Kaur, S., Lanham, P., Morant, N., Richards, J., Shah, P., Sutton, H., Vicary, R., Weaver, A., Wilks, J., Williams, M., Taylor, R. S. & Byford, S. (2015). Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. The Lancet, 386(9988), 63-73.
Jaurequi, M. E., Kimmes, J. G., Seibert, G. S., Ledermann, T., & Roberts, K. (2023). The role of mindfulness between adult attachment and anxiety: A dyadic approach. Couple and Family Psychology: Research and Practice, 12(3), 132–145.
Lindsay, E. K., Young, S., & Creswell, J. D. (2025). Mindfulness training fosters a positive outlook during acute stress: A randomized controlled trial. Emotion, 25(4), 815–826.
Mindfulness Based Cognitive Therapy. (n.d.). Retrieved 2022, February 17, from: https://mbct.co.uk/about-mbct/
Parra-Delgado, M., & Latorre-Postigo, J. M. (2013). Effectiveness of mindfulness-based cognitive therapy in the treatment of fibromyalgia: A randomised trial. Cognitive therapy and research, 37(5), 1015-1026.
Pseftogianni, F., Panagioti, M., Birtwell, K., & Angelakis, I. (2023). Mindfulness interventions for obsessive–compulsive and related disorders: A systematic review and meta-analysis of randomized controlled trials. Clinical Psychology Review, 233-243. https://doi.org/10.1037/cps0000132
Taylor, B. L., Strauss, C., Cavanagh, K., & Jones, F. (2014). The effectiveness of self-help mindfulness-based cognitive therapy in a student sample: a randomised controlled trial. Behaviour Research and Therapy, 63, 63-69.
Tickell, A., Ball, S., Bernard, P., Kuyken, W., Marx, R., Pack, S., Strauss, C., Sweeney, T. & Crane, C. (2020). The effectiveness of mindfulness-based cognitive therapy (MBCT) in real-world healthcare services. Mindfulness, 11(2), 279-290.