Cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT) are two therapeutic approaches that share some similarities but also have distinct differences.
CBT and DBT are both effective forms of therapy but differ in their target populations, philosophical underpinnings, and treatment emphasis.

Understanding these differences is important to ensure that individuals receive the most appropriate treatment based on their needs. This article will outline the similarities and differences between these two therapies.
What Is the difference between CBT and DBT?
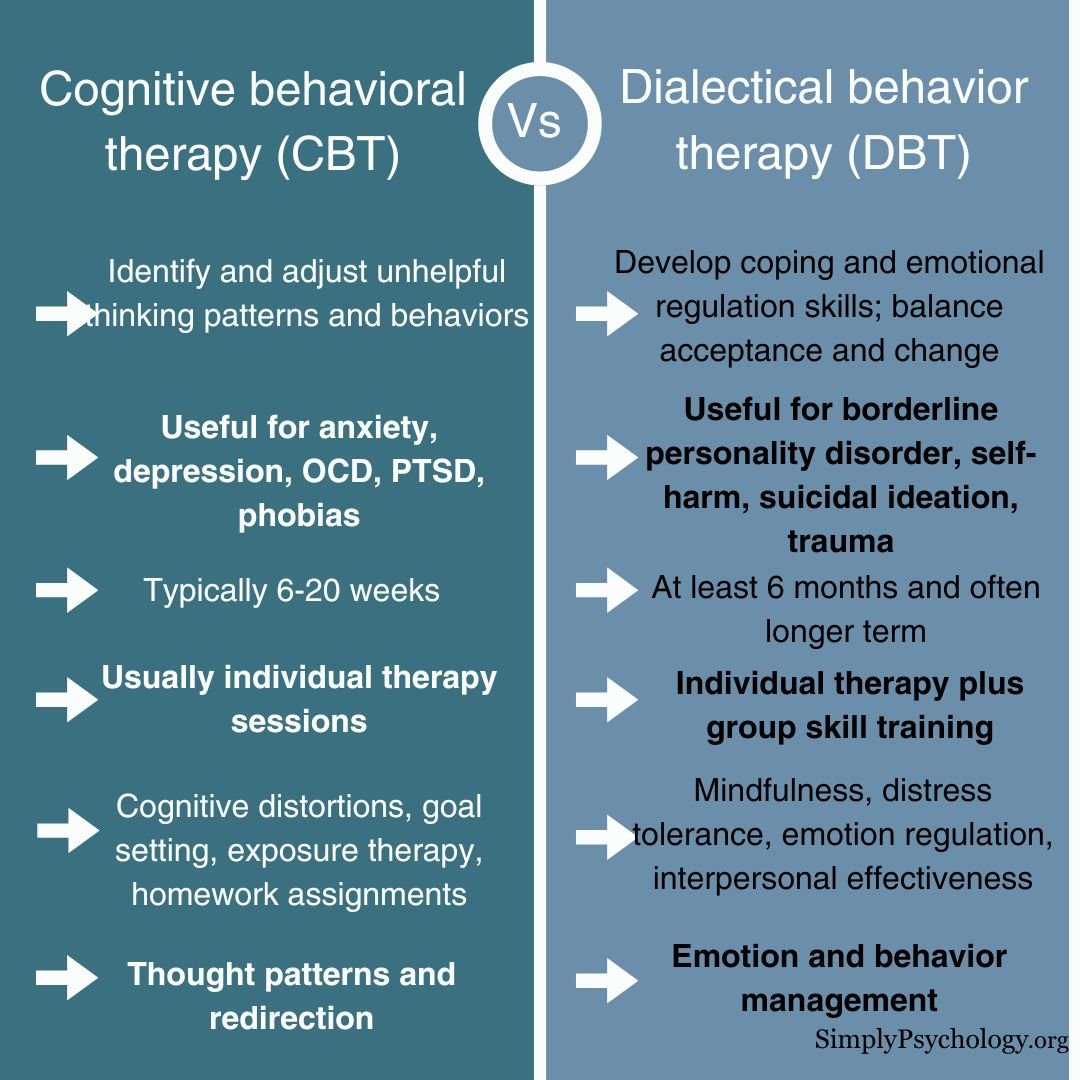
Cognitive behavioral therapy (CBT) identifies and challenges negative thought patterns to change behaviors and emotional responses. Dialectical behavior therapy (DBT), a form of CBT, emphasizes acceptance and change, teaching coping mechanisms for emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness.
While both target behavior and thought, DBT places a stronger emphasis on emotional regulation and interpersonal relationships.

Difference in emphasis
Both CBT and DBT ultimately aim to help the client change their thought patterns; however, CBT focuses more heavily on thought patterns and their redirection compared to DBT.
CBT helps people to identify when they are using cognitive distortions such as catastrophizing, mental filtering, overgeneralization, and learning to drop these types of thinking.
DBT places more emphasis on balance and the relationship between acceptance and change. In DBT, there is not a heavy reliance on changing thoughts.
Rather, the client is more mindful and accepting as they validate themselves in reality, but it is not the active, challenging process that happens in CBT.
Difference in time
CBT is usually completed after a short amount of time. The sessions will focus on specific problems with set goals in mind, so there is something to work towards.
CBT will usually finish once clients reach their goals which are typically within 6 to 20 weeks. DBT, on the other hand, usually involves sessions over a longer period of time where the therapist can consider the whole picture and help the client work through several issues.
DBT will often take at least six months to complete all the modules and can even last years in some instances.
Difference in practice
CBT nearly always takes place in a one-on-one setting with the therapist. The client and therapist work together for the session, and then the client will often have homework to take home.
In addition to individual weekly sessions, most DBT treatment also features a weekly group therapy component.
In these group sessions, people learn skills from one of the four modules and practice these skills as group settings offer a safe and supportive environment to complete this.
Differences in the kind of change created
CBT helps clients recognize and change their problematic patterns of thinking and behavior to have a healthier and more realistic outlook on life.
DBT helps clients regulate their intense emotions and improve interpersonal relationships through validation, acceptance, and behavioral changes.
Difference in suitability
There is a difference in how suitable each therapy is for improving the symptoms of mental health conditions. For depression, anxiety, obsessive-compulsive disorder (OCD), phobias, and posttraumatic stress disorder (PTSD), research has shown that CBT tends to be the more effective treatment.
In comparison, DBT tends to be better suited to those with BPD, self-harming behaviors, and chronic suicidal ideation.
What is cognitive behavioral therapy?
Cognitive behavioral therapy (CBT) is a widely used type of psychotherapy that helps people to identify their unhelpful thinking patterns and behaviors, then work together with the therapist to restructure these into healthier thoughts and behaviors.

CBT emerged in the 1960s in the work of psychiatrist Aaron Beck, who noted that certain types of thinking contributed to emotional problems – which were labeled automatic negative thoughts.
People commonly seek CBT for help in treating anxiety disorders and depression, but it can be helpful for several other mental health disorders or any mental distress.
CBT focuses on changing the automatic negative thoughts contributing to and worsening emotional difficulties, depression, and anxiety.
What is the idea behind CBT?
CBT is based on the idea that how we think (cognition), how we feel (emotion), and how we act (behavior) all interact together.
Therefore, negative and unrealistic thoughts can result in feelings of distress and, in turn, have a negative impact on actions.
CBT aims to help people become aware of when they make negative interpretations and behavioral patterns and helps to develop alternative ways of thinking and behaving to reduce psychological distress.
What are some techniques used in CBT?
Identifying negative thoughts – this involves learning about how an individual’s thoughts, feelings, and situations can contribute to maladaptive behaviors.
Practicing new skills can involve practicing coping skills and rehearsing them with the therapist to use in real-life situations.
Goal setting – this is an important step in recovery. The therapist teaches the individual how to identify their goals, distinguish between short- and long-term goals, and focus on the process as much as the end outcomes.
Problem-solving – CBT can help people identify and solve problems that arise from life stressors and reduce the negative impact of psychological and physical illness.
Self-monitoring – this can be done through diary work – tracking behaviors, symptoms, or experiences over time and sharing them with the therapist.
This can help provide the therapist with the information needed to provide the best treatment.
What is dialectical behavioral therapy?
Dialectical behavioral therapy (DBT) is a type of CBT originally intended to treat borderline personality disorder but has since been adapted to treat other conditions.
This type of therapy is used to help people who have difficulty regulating their emotions or are exhibiting self-destructive behaviors such as eating disorders, substance-use disorders, or those who exhibit self-harming behavior.
DBT helps to address thoughts and behaviors while incorporating strategies such as emotional regulation and mindfulness.
DBT aims to teach people how to develop healthy ways to cope with stress, regulate their emotions, and improve relationships with others. This therapy can help people who may lack useful coping skills and find that they move from one crisis to another.
Why was DBT developed?
Marsha Linehan developed DBT in the 1980s to help people with suicidal thoughts who often had a borderline personality disorder (BPD) diagnosis. Individuals with BPD often suffer from the following symptoms:
-
Experience intense emotions
-
Have difficulties with their relationships
-
Their actions are very impulsive
-
Their thinking is very black and white
Therefore, DBT was developed to help people with DBT manage these core symptoms by providing them with skills to reach their goals.
This way, people with BPD would know how to respond to challenging situations or manage relationships, to improve their quality of life overall.
What are some techniques used in DBT?
There are four modules that are covered in DBT:

Mindfulness – DBT teaches people to be focused on the present moment and feel grounded. This is especially useful for those struggling with an unstable sense of self and difficulties staying focused on the present.
After focusing on the present moment, the idea is that the automatic negative thoughts are not engaged with.
Emotion regulation – DBT helps people learn how to manage their emotions so that intense emotions do not end up controlling the situation.
They learn that they can choose how to react to negative/strong emotions. They can also learn to avoid situations that they know will trigger strong emotions.
Distress tolerance – DBT teaches people how to manage upsetting situations, such as helping them to think about some of the healthy things they can do to manage their behavior and emotions so that they do not act impulsively or risky.
Interpersonal effectiveness – DBT aims to teach people to communicate in healthy and respectable ways. It can teach assertiveness and how to set healthy boundaries with others. It can build listening skills and conflict resolution skills and help to build trust with others.
What can CBT and DBT Help With?
CBT is used to treat a range of conditions, including:
-
Bipolar disorder
-
Addiction
-
Anger
-
Eating disorders
-
Phobias
-
Personality disorders
Aside from mental health conditions, CBT has also been used to help people cope with the following:
-
Chronic pain
-
Divorce or breakups
-
Grief
-
Insomnia
-
Relationship problems
Although DBT was developed with borderline personality disorder in mind, the techniques used in DBT can be effective for many of the following mental health conditions:
-
Depression
-
Bipolar disorder
-
PTSD
-
Eating disorders
-
Substance-use disorders
Aside from mental health conditions, DBT has also been used to help people cope with the following:
-
Intense emotions
-
Managing challenging situations
-
Relationship difficulties
-
Self-injurious behavior and suicidal ideation
-
Extreme stress
CBT and DBT have shown to be very helpful for various issues. Some of the notable benefits include:
-
Improving communication skills
-
Healthier thinking patterns and a greater awareness of negative thoughts
-
Improved ability to make healthier choices
-
Greater insights into one’s own life
-
Improved coping strategies to manage distress
-
Being able to view situations from another perspective
-
Helping people to move toward a solution
-
Learning more about one’s own goals and values
-
Developing skills for facing challenges in the present and in the future
Effectiveness of CBT
CBT is one of the most researched therapy types, partly because treatment focuses on highly specific goals, and results can be measured relatively easily.
-
Meta-analyses have found that CBT is strongly effective, especially in improving the symptoms in people with anxiety-related disorders, including OCD and PTSD, as well as in anger problems, drug abuse, and general stress (Hofman et al., 2012).
-
Another meta-analysis found that CBT is a moderately effective treatment for anxiety disorders when compared to a placebo (Carpenter et al., 2018).
-
As well as face-to-face sessions, CBT has been found to be as effective as online sessions (Kumar et al., 2017).
-
CBT has also been used with children and adolescents, with findings suggesting that this therapy can be effective in treating symptoms of depression and anxiety in these age groups (Oud et al., 2019).
-
An analysis of CBT for insomnia supports the effectiveness of this treatment and for the prevention of relapse of primary insomnia (Okajima et al., 2011).
Effectiveness of DBT
-
Linehan et al. (1991) conducted the first randomized controlled trial of the effectiveness of DBT on women with BPD. It was found that after completion of DBT, participants showed significant improvements in chronically suicidal and self-injurious behaviors.
-
A more recent meta-analysis of the effectiveness of DBT on those with diagnosed BPD found that most studies reported significant reductions in suicidal ideation, self-injurious behavior, depression, and anxiety (Bloom et al., 2012).
-
Since its introduction, DBT continues to be an effective psychotherapy for BPD, with one study finding that after a year of therapy, around 77% of patients no longer met the criteria for the diagnosis of BPD (Stiglmayr et al., 2014).
-
DBT is often recommended as a first-line treatment of BPD and has been shown to reduce the need for medical care and medication by as much as 90% (May et al., 2016).
-
As well as being effective for BPD, there is also evidence that the skills learned in DBT reduced depressive symptoms, improved affective control, and improved the mindfulness self-efficacy of those with bipolar disorder (Van Dijk et al., 2013).
-
DBT has also been shown to help treat some of the symptoms associated with post-traumatic stress disorder (PTSD). It was found in a study that after completion of the therapy, individuals with PTSD were less likely to attempt suicide and self-harm and had reduced feelings of shame, anxiety, and trauma-related guilt (Harned et al., 2014).
Are CBT and DBT my Only Options?
While CBT and DBT have proven effective for many conditions, they do not represent the only options for mental health treatment. Likewise, these types of therapy may not work for everyone.
Other forms of therapy focus more heavily on managing trauma, improving relationships, discovering inner strengths, and additional areas.
For example, acceptance and commitment therapy (ACT) utilizes acceptance, mindfulness, and values to foster psychological flexibility. Eye movement desensitization and reprocessing (EMDR) specifically treats trauma and distressing memories.
Additionally, factors like a strong patient-therapist alliance can influence outcomes regardless of the techniques used. An openness to new perspectives and a willingness to try various approaches may aid in finding what works best for each individual.
If CBT or DBT do not seem the right fit, exploring alternatives could uncover better-suited treatment. One form of therapy does not universally apply to all people and situations.
Related Articles
References
Dissociative Disorders. (Jul 05, 2021). 2021 Traumadissociation.com. Retrieved Jul 5, from http://traumadissociation.com/dissociative.
Dissociative Identity Disorder. (Jul 05, 2021). Traumadissociation.com, Retrieved Jul 5, 2021, from h
Bloom, J. M., Woodward, E. N., Susmaras, T., & Pantalone, D. W. (2012). Use of dialectical behavior therapy in inpatient treatment of borderline personality disorder: a systematic review. Psychiatric Services, 63(9), 881-888.
Carpenter, J. K., Andrews, L. A., Witcraft, S. M., Powers, M. B., Smits, J. A., & Hofmann, S. G. (2018). Cognitive behavioral therapy for anxiety and related disorders: A meta‐analysis of randomized placebo‐controlled trials. Depression and anxiety, 35(6), 502-514.
Harned, M. S., Korslund, K. E., & Linehan, M. M. (2014). A pilot randomized controlled trial of Dialectical Behavior Therapy with and without the Dialectical Behavior Therapy Prolonged Exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behaviour research and therapy, 55, 7-17.
Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive therapy and research, 36(5), 427-440.
Kumar, V., Sattar, Y., Bseiso, A., Khan, S., & Rutkofsky, I. H. (2017). The effectiveness of internet-based cognitive behavioral therapy in treatment of psychiatric disorders. Cureus, 9(8).
Linehan, M. M., Armstrong, H. E., Suarez, A., Allmon, D., & Heard, H. L. (1991). Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of general psychiatry, 48(12), 1060-1064.
May, J. M., Richardi, T. M., & Barth, K. S. (2016). Dialectical behavior therapy as treatment for borderline personality disorder. Mental Health Clinician, 6(2), 62-67.
Okajima, I., Komada, Y., & Inoue, Y. (2011). A meta-analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomnia. Sleep and biological rhythms, 9(1), 24-34.
Oud, M., De Winter, L., Vermeulen-Smit, E., Bodden, D., Nauta, M., Stone, L., van den Heuvel, M., Al Taher, R., de Graaf, I., Kendall, T., Engels, R. & Stikkelbroek, Y. (2019). Effectiveness of CBT for children and adolescents with depression: A systematic review and meta-regression analysis. European psychiatry, 57, 33-45.
Stiglmayr, C., Stecher-Mohr, J., Wagner, T., Meiβner, J., Spretz, D., Steffens, C., Roepke, S., Fydrich, T., Salbach-Andrae, H., Schulze, J. & Renneberg, B. (2014). Effectiveness of dialectic behavioral therapy in routine outpatient care: the Berlin Borderline Study. Borderline personality disorder and emotion dysregulation, 1(1), 1-11.
Van Dijk, S., Jeffrey, J., & Katz, M. R. (2013). A randomized, controlled, pilot study of dialectical behavior therapy skills in a psychoeducational group for individuals with bipolar disorder. Journal of affective disorders, 145(3), 386-393.