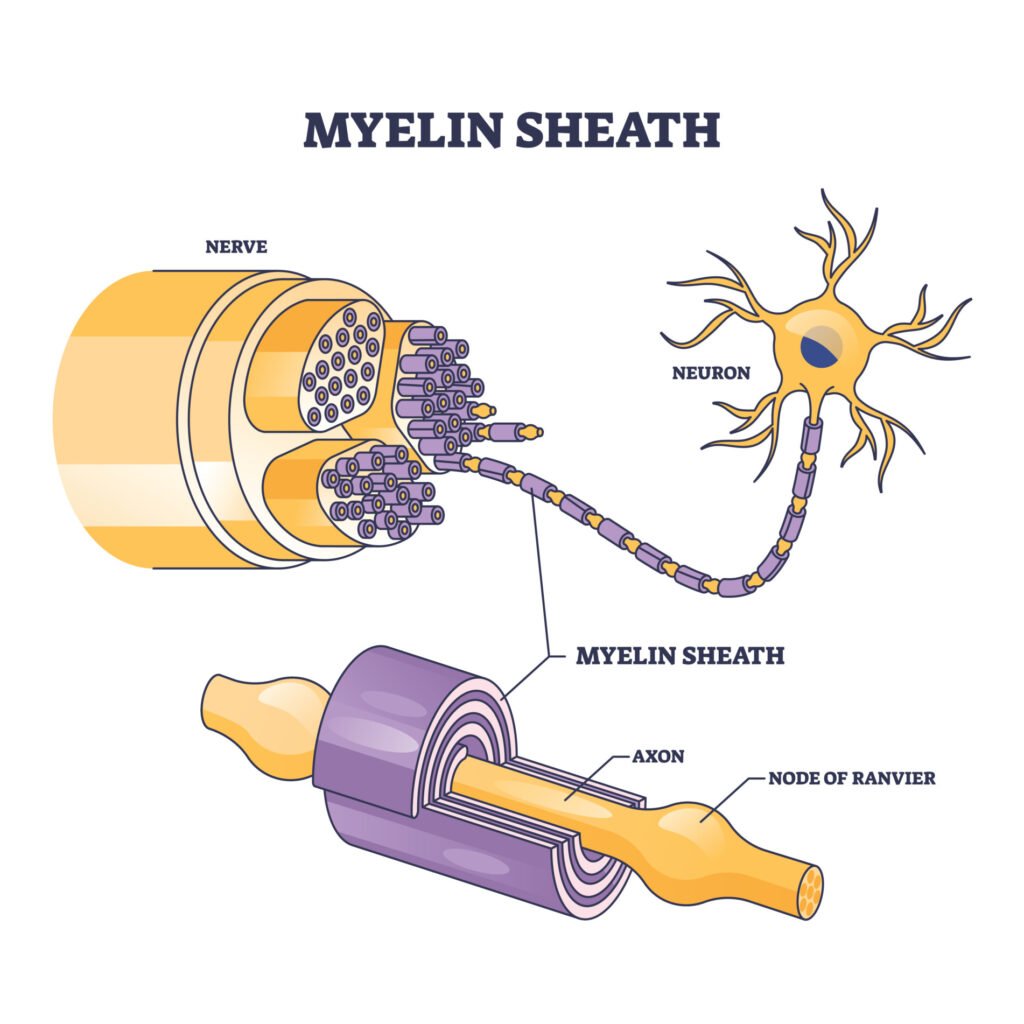
Demyelination is the loss or damage to the myelin sheath, the protective covering that surrounds nerve fibers and allows signals to be quickly and efficiently conducted along neurons.
When myelin is damaged or stripped away, neuronal signaling slows, leading to impaired sensation, movement, cognition, or other nervous system functions.
This loss impairs efficient electrical signal transmission along the neuron, potentially leading to neurological symptoms.
Disorders such as multiple sclerosis are characterized by demyelination, causing symptoms ranging from muscle weakness to impaired coordination or vision.

Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of a qualified healthcare provider with any questions you may have about a medical condition.
Why is Myelin Important?
Imagine trying to stream a video with a frayed internet cable. The signal cuts in and out. Similarly, when myelin is damaged, nerves can’t transmit signals efficiently.
Myelin allows for fast, reliable communication between the brain, spinal cord, and body.
Damage to this layer causes delays or complete blockages in nerve signaling, which can lead to physical and mental symptoms such as muscle weakness, numbness, or cognitive difficulties.
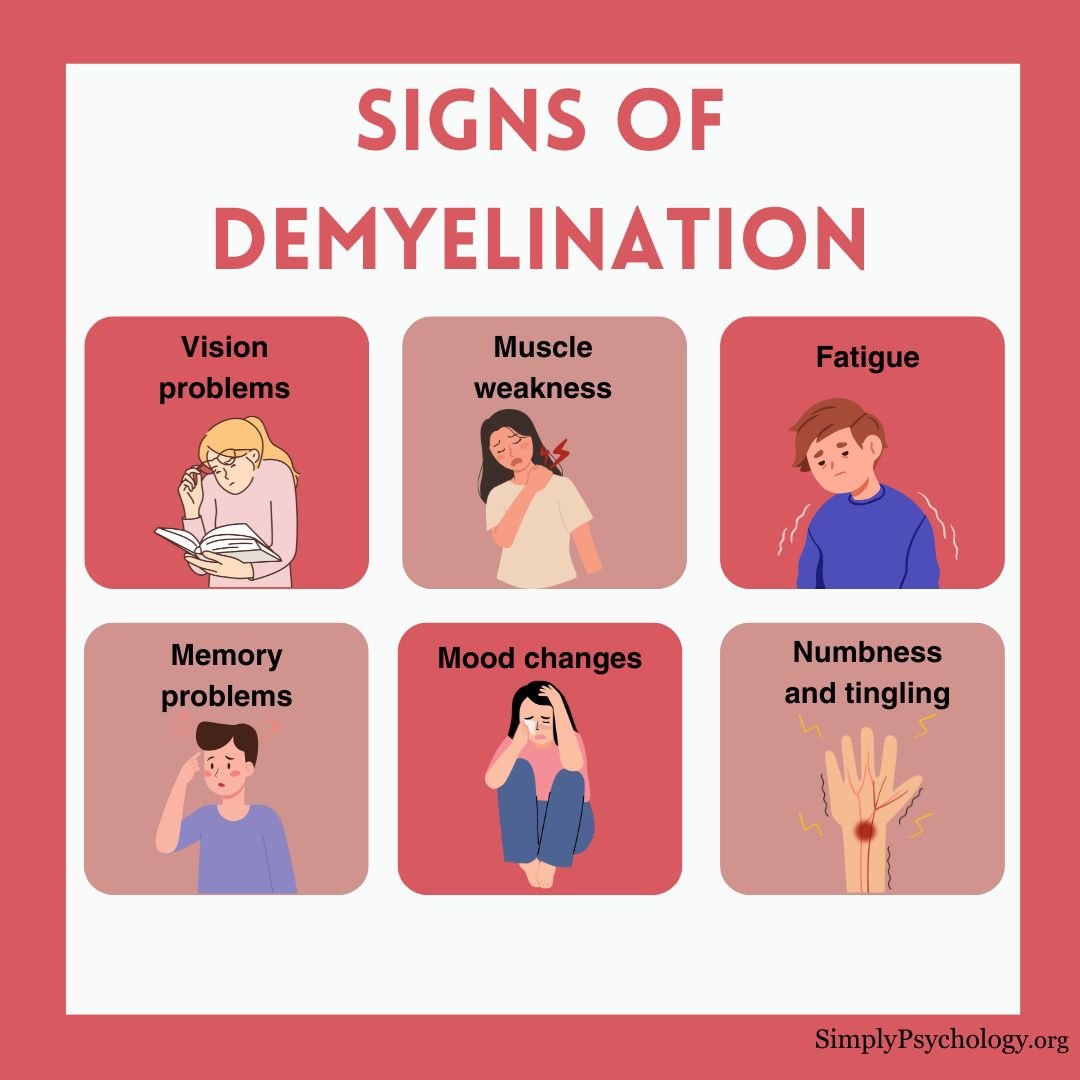
Signs of demyelination
The symptoms of demyelination depend on the condition and where in the nervous system the demyelination has occurred.
The symptoms of demyelination correspond to the area of the nervous system affected. For instance, peripheral neuropathy affects the hands and feet.
Not everyone who is affected by demyelination has the same symptoms, although some are very common. Early signs that are among the first symptoms of demyelination include:
- Sudden vision loss or blurred vision
- Tingling or numbness in limbs
- Fatigue that doesn’t improve with rest
- Muscle weakness or poor coordination
- Unusual nerve pain
- Bladder or bowel dysfunction

Below are some of the common areas where demyelination can cause impairments and how they affect different parts of the nervous system:
Vision
Demyelinating conditions can lead to blurry or double vision. They can also result in a loss of vision that can be either temporary or permanent, depending on the severity of the demyelination.
Reflexes and movement
Demyelination can cause changes to the motor system which can lead to muscle weakness, stiffness, uncoordinated movements, and problems with balance.
This can ultimately affect how someone moves, meaning that they may not be able to perform some motor tasks or find it harder to walk, speak, or swallow.
Sensations
Those with demyelinating conditions may experience numbness and tingling, burning, or prickling sensations in their arms, legs, or feet.
In some cases, they may even feel pain when touched lightly, which can make it extremely difficult to navigate life as normal.
Cerebellum
The cerebellum is a part of the brain that plays a role in controlling balance and coordination. Demyelination in this area can lead to tremors or incoordination such as finding it harder to walk without losing balance.
Genitourinary system
Some people with demyelinating conditions may experience problems with urination and bowel movements. This can also affect sexual health and make someone more likely to develop a urinary tract infection (UTI).
Mood and thinking
There may be changes in mood associated with demyelination, such as many experiencing depression, anxiety, and irritability.
There may also be problems with thinking, such as memory issues and a loss of focus, with some taking longer to process their thoughts.
Blood pressure and heart
In some cases, demyelination may result in people having poorer control over their blood pressure, as well as having a racing heartbeat or palpitations with no apparent cause.
What causes demyelination?
Demyelination can result from various factors, including immune system attacks, infections, or environmental and genetic influences.
Primary causes include:
- Autoimmune reactions: Conditions like multiple sclerosis (MS) occur when the immune system mistakenly attacks myelin.
- Viral infections: Viruses such as the JC virus may trigger demyelination, especially in those with weakened immune systems.
- Genetics: Some inherited disorders, like leukodystrophies, affect myelin production.
Other contributing factors:
- Reduced oxygen to the brain
- Vitamin deficiencies (e.g., B12)
- Exposure to toxins or heavy metals
- Chronic alcoholism or liver damage
- Vascular diseases and inflammation
Demyelinating Disorders
Several neurological disorders are caused by or associated with demyelination:
Multiple Sclerosis (MS)
MS is the most well-known demyelinating condition. It affects the brain, spinal cord, and optic nerves. In MS, immune cells damage myelin, leading to scarring and disrupted nerve signaling.
People with MS may experience fluctuating symptoms such as numbness, vision problems, fatigue, or difficulty walking. It typically follows a relapsing-remitting or progressive course.

Guillain-Barré Syndrome (GBS)
GBS involves rapid-onset muscle weakness due to immune attacks on peripheral nerves. It’s often triggered by infections and may progress quickly but can be treatable with early intervention.
Optic Neuritis
This condition causes inflammation of the optic nerve, often leading to pain and temporary vision loss in one eye. It can be an early sign of MS.
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
CIDP is a rare, long-term condition where immune cells attack peripheral nerve myelin. It causes gradual weakness, numbness, and sensory loss, especially in the limbs.
How Is Demyelination Diagnosed?
Diagnosing demyelination involves a combination of clinical evaluation and diagnostic tests:
- Neurological exam: Doctors assess reflexes, strength, coordination, and sensory function.
- MRI scans: Used to detect lesions or inflammation in the brain and spinal cord.
- Lumbar puncture: Analyzes cerebrospinal fluid for markers of inflammation or infection.
- Blood tests: Rule out vitamin deficiencies or autoimmune markers.
- Evoked potentials: Measure how quickly electrical signals move through the nervous system.
Early diagnosis is crucial for managing symptoms and preventing long-term damage.
Treatment
While myelin damage can’t always be reversed, treatments can slow progression, reduce inflammation, and improve symptoms.
Treatment strategies include:
- Medications: Corticosteroids reduce inflammation; disease-modifying therapies (DMTs) are used in MS.
- Plasma exchange (plasmapheresis): Removes harmful antibodies from the blood, often used in GBS or severe relapses.
- Immunoglobulin therapy: Provides antibodies that modulate the immune response.
- Physical therapy: Helps maintain strength, flexibility, and function.
- Vitamin supplementation: Especially important for deficiencies such as B12.
Living with Demyelination
A diagnosis of a demyelinating condition can be overwhelming, but many people manage symptoms successfully with treatment and support. Regular follow-ups, symptom tracking, and healthy lifestyle choices can make a significant difference.
Support groups, counseling, and patient education also play vital roles in managing the emotional and psychological impact of chronic neurological conditions.
References
Railton, D. (2021, November 28). What is demyelination, and what causes it? Medical News Today. https://www.medicalnewstoday.com/articles/318750
Apetauerova, D. (2021, September 20). An Overview of Demyelination. Very Well Health. https://www.verywellhealth.com/demyelination-4691934#toc-causes
Healthline Editorial Team. (2019, October 1). Demyelination: What Is It and Why Does It Happen? Healthline. https://www.healthline.com/health/multiple-sclerosis/demyelination
Reiff Ellis, R. (2020, August 9). What Are Demyelinating Diseases? WebMD. https://www.webmd.com/multiple-sclerosis/what-are-demyelinating-disorders
National Multiple Sclerosis Society. (n.d.) Understanding MS. Retrieved 2022, January 10, from https://www.nationalmssociety.org/What-is-MS/MS-FAQ-s
Centers for Disease Control and Prevention. (2019, December 20). Guillain-Barré Syndrome. https://www.cdc.gov/campylobacter/guillain-barre.html

