The HPA axis, or hypothalamic-pituitary-adrenal axis, is a complex set of interactions between the hypothalamus, pituitary gland, and adrenal glands.
It plays a critical role in regulating stress responses, mood, digestion, immune function, and energy storage and expenditure in the body.
The pathway of the axis results in the production of cortisol.
The stress response aims to provide energy for an extended period of time. It does not need to be fast, so it uses hormones to transmit signals.

Key Takeaways
- The HPA axis is a hormone-based communication system between your brain and adrenal glands that regulates stress, energy, and mood.
- When you face a stressor, the HPA axis activates to release cortisol and help your body cope with prolonged demands.
- Dysfunction in this system—often caused by chronic stress or trauma—can lead to fatigue, anxiety, depression, and immune issues.
- Conditions like Cushing syndrome, PTSD, and alcohol dependence are closely linked to abnormal cortisol levels.
- Supporting your HPA axis involves a mix of medical treatment, therapy, exercise, proper sleep, and stress-reducing habits like meditation.
What Is the HPA Axis?
The HPA axis is a communication network that links your brain to your adrenal glands. It includes three main parts:
- Hypothalamus: Located at the base of the brain, it detects stress and releases a hormone called corticotropin-releasing hormone (CRH).
- Pituitary Gland: Triggered by CRH, it sends out adrenocorticotropic hormone (ACTH).
- Adrenal Glands: Sitting atop your kidneys, they respond to ACTH by releasing cortisol, the primary stress hormone.
Together, these organs help regulate stress, energy levels, digestion, mood, and the immune system.
How Does the HPA Axis Work?
When your body encounters a stressor, it triggers two responses.
First, within seconds, the sympathetic nervous system releases epinephrine and norepinephrine, causing immediate physical changes like increased heart rate.
About 10 seconds later, the HPA axis activates, providing a longer-term stress response.
Imagine you’re about to give a presentation. Your body prepares in two stages:
- Immediate Response: Your sympathetic nervous system kicks in, increasing your heart rate and alertness.
- Sustained Response: A few seconds later, the HPA axis activates, gradually releasing cortisol to maintain energy and focus.
HPA Axis and the Fight-or-Flight Response
The fight-or-flight response has two parts. The sympathetic-adrenal-medullary (SAM) system triggers the body’s immediate reaction to danger—releasing adrenaline and noradrenaline within seconds to increase heart rate and alertness.
The HPA axis, in contrast, kicks in a little later. It releases cortisol to help the body sustain energy, focus, and vigilance during prolonged stress. Together, these systems coordinate your full biological response to threats.

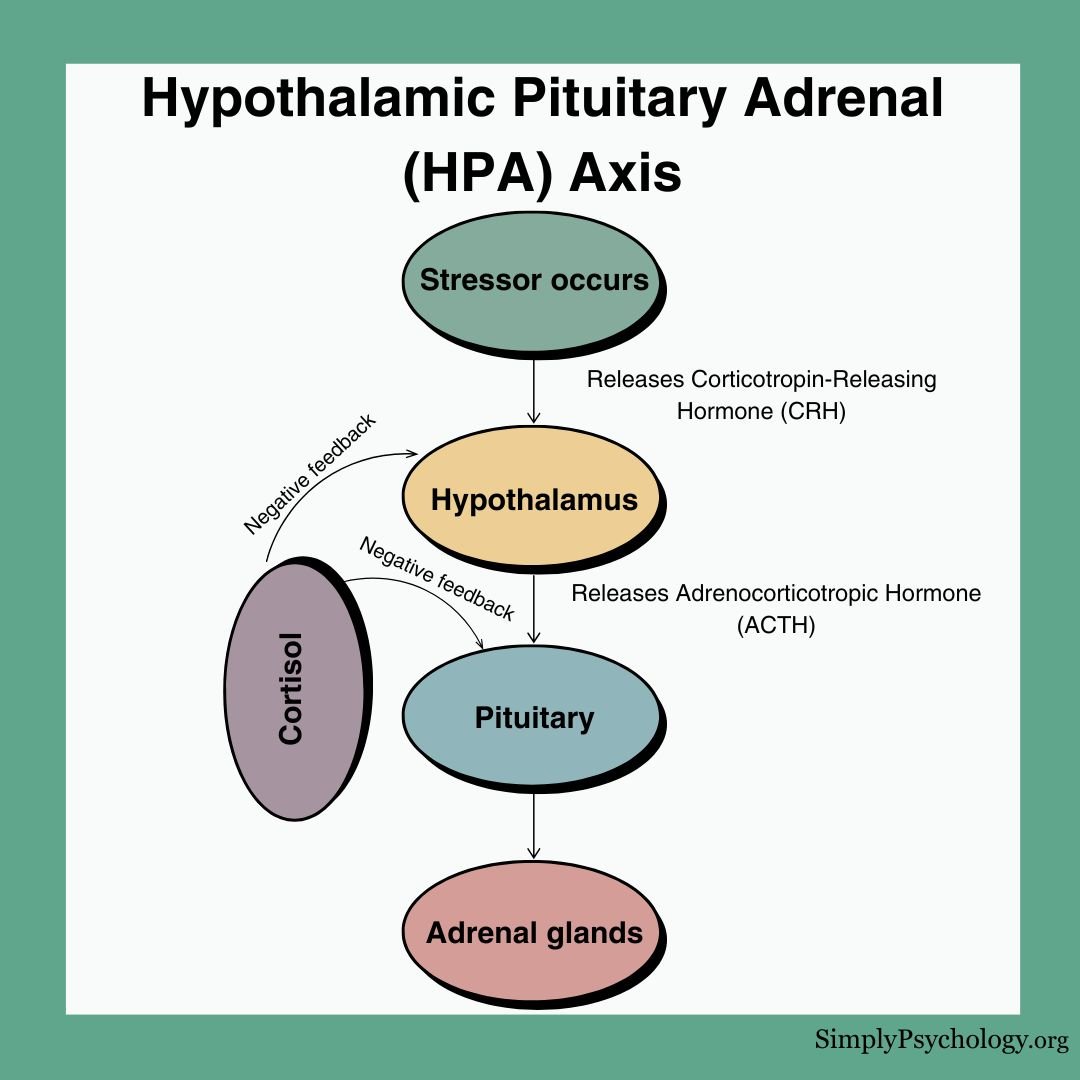
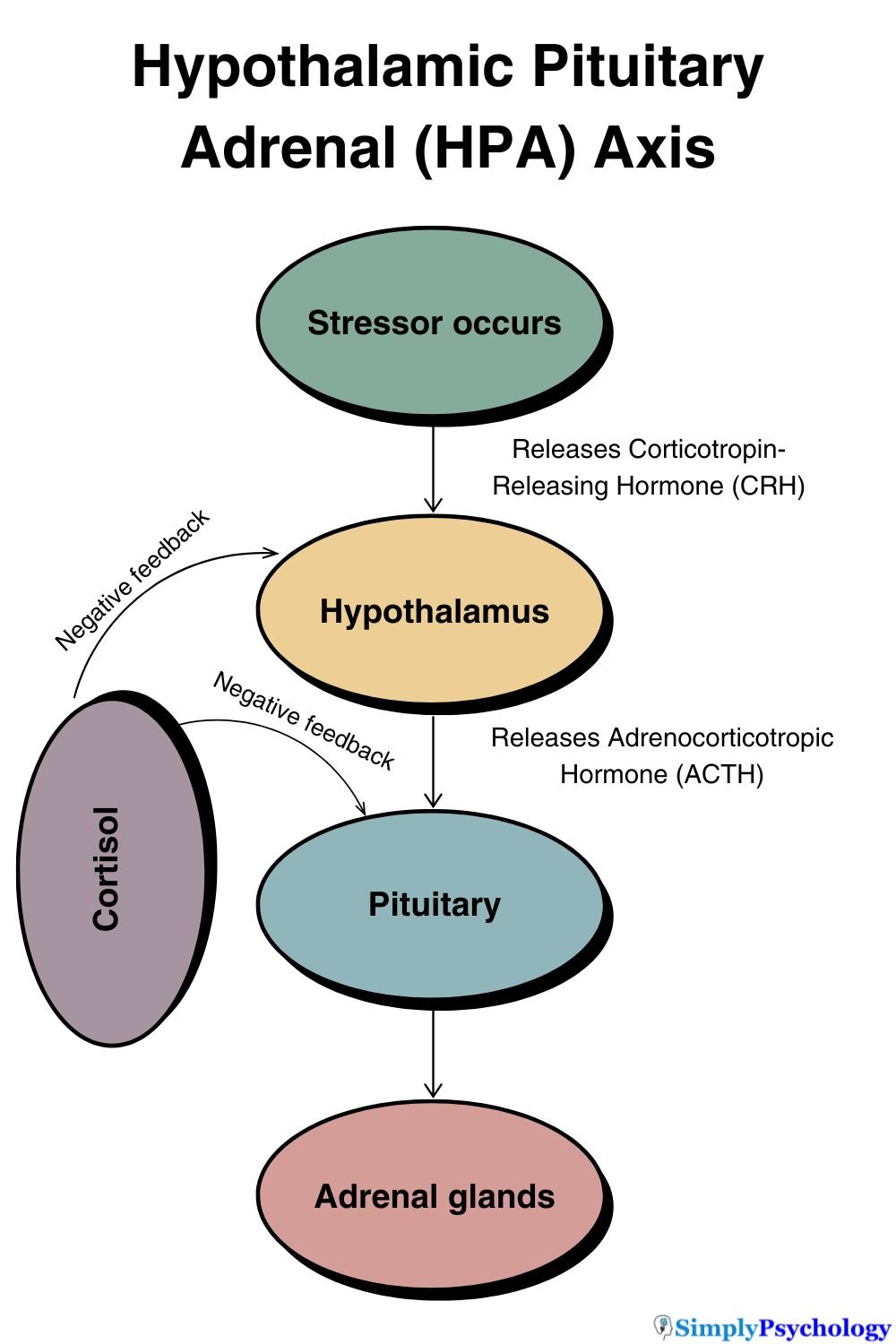
The HPA axis follows a cascade of hormone releases:
- The hypothalamus releases Corticotropin-Releasing Hormone (CRH), the main regulator of the stress response.
- CRH travels to the anterior pituitary gland, triggering it to release Adrenocorticotropic Hormone (ACTH) into the bloodstream.
- ACTH reaches the adrenal glands and binds to the outer layer (adrenal cortex), specifically the zona fasciculata region.
- The adrenal cortex then produces and releases cortisol into the bloodstream.
Cortisol and the Negative Feedback Loop
The HPA axis uses a negative feedback loop to maintain homeostasis—your body’s internal balance. When cortisol levels rise, receptors in the hypothalamus and hippocampus detect the increase and signal the system to stop producing more. This prevents overstimulation and helps your body return to a steady state after stress.
HPA Axis Dysfunction
Sometimes, chronic stress, trauma, or certain medications can disrupt the HPA axis. This dysfunction affects how your body produces and regulates cortisol.
Common Signs of Imbalance:
- Persistent fatigue
- Difficulty coping with stress
- Mood swings or irritability
- Trouble sleeping or concentrating
- Weakened immune system
Health Conditions Linked to HPA Dysregulation:
- Cushing Syndrome: Caused by too much cortisol, often due to prolonged steroid use or tumors.
- Depression and Anxiety: Irregular cortisol levels can affect brain regions involved in mood and memory.
- PTSD: Trauma can alter how the HPA axis responds to stress.
- Alcohol Dependence: Cortisol may interact with the brain’s reward system, increasing vulnerability to addiction.
Keeping the HPA Axis Regulating Normally
Maintaining balance in your HPA axis is essential for long-term physical and mental health. Here’s how to help your body stay regulated:
Medical Treatments:
- Medications for hormone-related conditions like Cushing syndrome
- Antidepressants or anti-anxiety drugs that normalize cortisol levels
Therapeutic Approaches:
- Cognitive Behavioral Therapy (CBT): Helps reframe stressful thoughts and improve resilience.
- Biofeedback: Teaches control over bodily stress responses using real-time feedback.
Lifestyle Changes That Help:
- Regular aerobic exercise
- Consistent sleep schedule
- Balanced diet to stabilize blood sugar
- Relaxation techniques like meditation, deep breathing, and yoga
Why the HPA Axis Matters
The HPA axis is more than a stress switch—it’s central to your health. When it’s working well, you feel energized, calm, and focused.
When it’s not, everyday challenges can feel overwhelming. By understanding and supporting this system, you can build resilience and improve both mental and physical well-being.
Practice Questions for Exam Revision
Use these questions to test your understanding of the HPA axis:
- Outline the role of the HPA axis in the stress response. (4 marks)
- Explain how the negative feedback loop helps regulate cortisol levels. (4 marks)
- Describe one physical and one psychological health consequence of HPA axis dysfunction. (6 marks)
- Compare the roles of the HPA axis and the SAM system in the stress response. (6 marks)
References
Guilliams, T. G., & Edwards, L. (2010). Chronic stress and the HPA axis. The standard, 9(2), 1-12.
Mayo Clinic. (2021, April 30). Cushing syndrome. https://www.mayoclinic.org/diseases-conditions/cushing-syndrome/symptoms-causes/syc-20351310
Moylan, S., Maes, M., Wray, N. R., & Berk, M. (2013). The neuroprogressive nature of major depressive disorder: pathways to disease evolution and resistance, and therapeutic implications. Molecular psychiatry, 18(5), 595-606.
Neuroscientifically Challenged. (2014, June 4). Know Your Brain: HPA Axis. https://www.neuroscientificallychallenged.com/blog/2014/5/31/what-is-the-hpa-axis
Newcomer, J. W., Selke, G., Melson, A. K., Hershey, T., Craft, S., Richards, K., & Alderson, A. L. (1999). Decreased memory performance in healthy humans induced by stress-level cortisol treatment. Archives of general psychiatry, 56(6), 527-533.
Smith, S. M., & Vale, W. W. (2006). The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues in clinical neuroscience, 8(4), 383.
Stephens, M. A. C., & Wand, G. (2012). Stress and the HPA axis: Role of glucocorticoids in alcohol dependence. Alcohol research: current reviews.