The limbic system is a complex network of interconnected brain structures that plays a pivotal role in regulating human behavior and emotion, especially those tied to survival instincts.
It also contributes significantly to the processing of memory and motivation.
This neural system encompasses the amygdala, hippocampus, thalamus, hypothalamus.
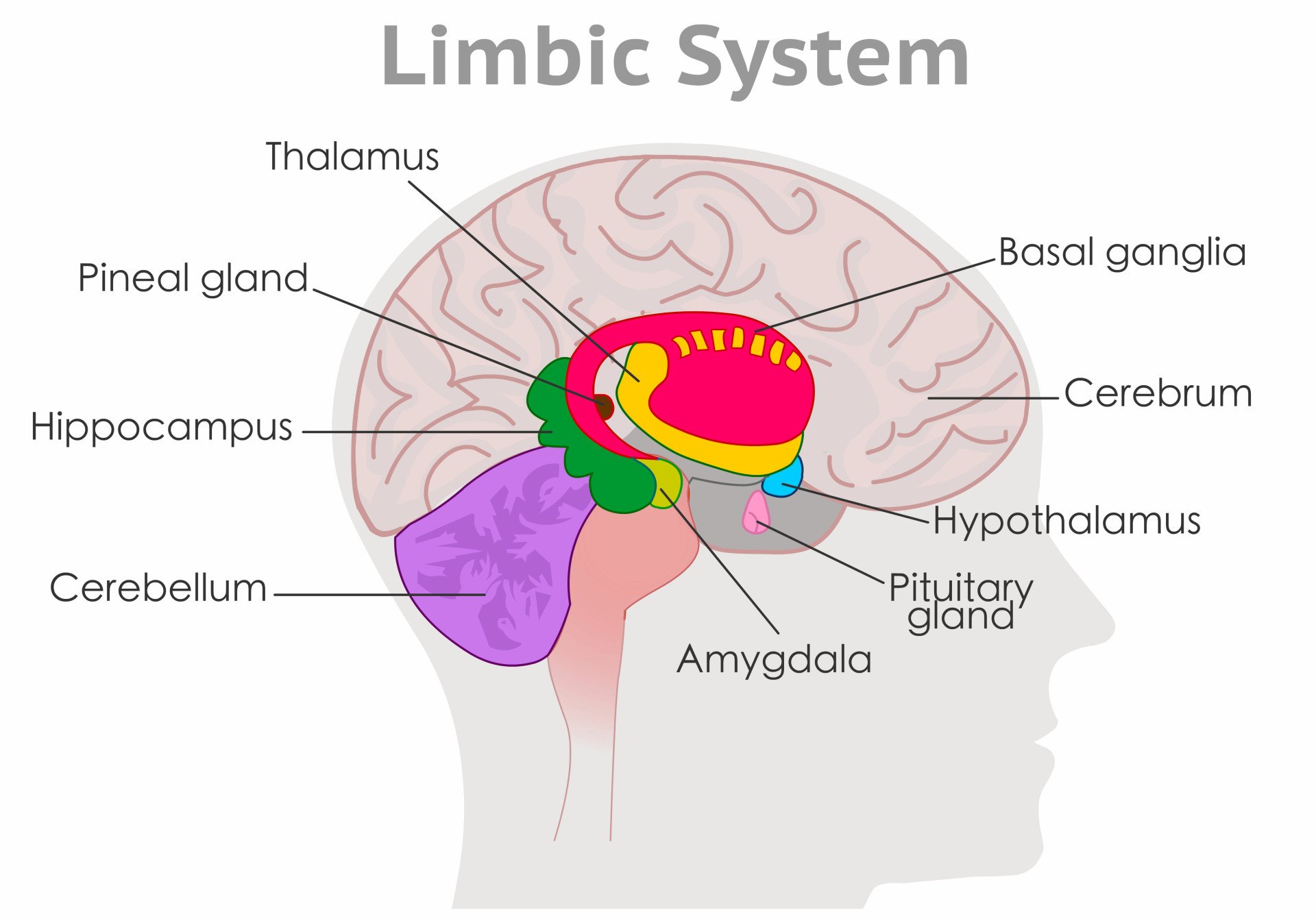
Structural Components
This neural system encompasses several specialized structures working in coordination:
- Amygdala: Primarily responsible for emotional processing, particularly those tied to survival instincts like fear and aggression.
- Hippocampus: Crucial for memory formation and the consolidation of short-term memory into long-term storage.
- Hypothalamus: Acts as the link to the endocrine system; it regulates essential physiological functions such as feeding, reproduction, and the stress response.
- Thalamus: Functions as a relay station, channelling sensory information to the appropriate limbic and cortical areas for processing.
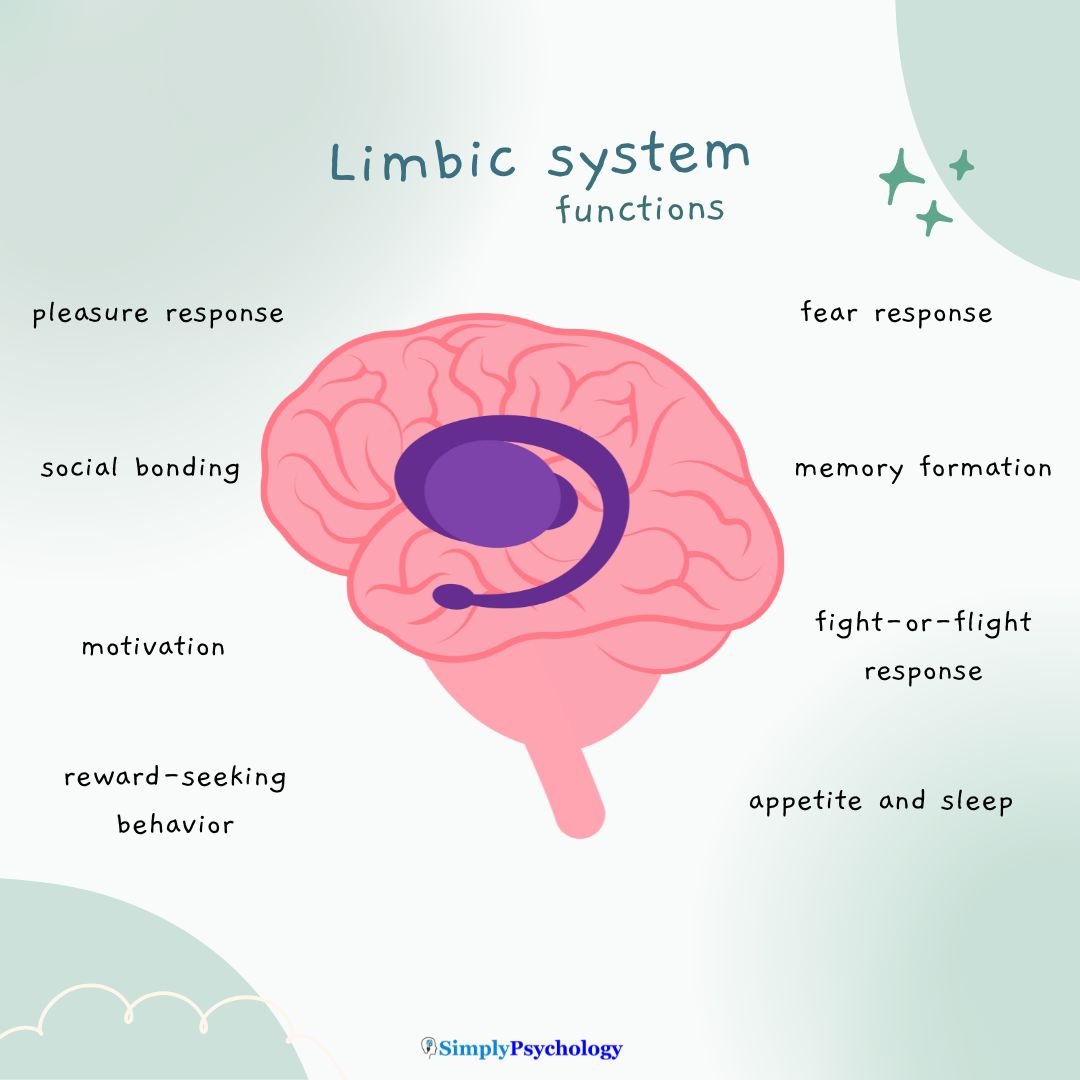
Functions
The limbic system manages responses tied to survival and social interaction through several pathways:
- Emotional Processing: Coordinates responses to stimuli, including social bonding and the fight or flight response.
- Memory and Learning: Integrates current sensations with past memories to guide future behavior.
- Motivation and Reward: Drives behaviors essential for survival, such as seeking food or avoiding danger.
- Physiological Homeostasis: Works with the autonomic nervous system to regulate heart rate, blood pressure, and stress hormones during emotional states.
Where Is the Limbic System Located?
The limbic system lies beneath the cerebral cortex and surrounds the top of the brainstem.
It’s tucked deep within the brain, mainly in the temporal lobes, and includes older, evolutionarily conserved structures.
Unlike the neocortex, which has six layers of cells, parts of the limbic system have fewer layers.
This simpler structure supports faster, more instinctual processing.
Main Structures of the Limbic System
The limbic system is made up of several interconnected brain structures, each playing a unique role in emotion, memory, and motivation.
Here’s a closer look at its key parts:
Hippocampus
- Converts short-term experiences into long-term memories, especially episodic and spatial memory.
- Supports learning, especially when emotions are involved.
- Works closely with the prefrontal cortex to help recall past experiences for decision-making.
- Has strong connections with the amygdala, linking emotions to memories (e.g., remembering emotionally intense events more vividly).
- One of the few brain areas where neurogenesis continues into adulthood, possibly supporting emotional resilience.
Clinical insight: Hippocampal damage is linked to amnesia, disorientation, and memory loss, and plays a role in Alzheimer’s disease, dementia, and post-stroke cognitive decline.
Amygdala
- Detects emotional stimuli and triggers rapid responses, especially for fear, anger, and threat detection.
- Attaches emotional salience to memories, helping prioritize what we remember.
- Plays a key role in fear learning, especially through repetition of threatening experiences.
- Connects to the hypothalamus and autonomic nervous system, initiating the body’s fight-or-flight response.
- Also involved in social behavior, such as recognizing facial expressions and emotional cues.
Clinical link: Abnormal amygdala function is linked to anxiety disorders, PTSD, borderline personality disorder, and even psychopathy.
Hypothalamus
- Maintains homeostasis by controlling hunger, thirst, sleep, body temperature, and circadian rhythms.
- Regulates hormonal responses by signaling the pituitary gland, acting as the bridge between the brain and endocrine system.
- Plays a critical role in sexual behavior, maternal bonding, and aggression.
- Initiates the stress response by activating the hypothalamic-pituitary-adrenal (HPA) axis.
Clinical relevance: Chronic dysregulation is associated with mood disorders, eating disorders, and chronic stress syndromes. Overactivity can lead to anxiety; underactivity can contribute to depression.
Cingulate Gyrus
- Involved in regulating emotions, especially in response to pain or distress.
- Helps monitor conflict and decision-making, particularly when there’s emotional uncertainty.
- Integrates emotional processing with motor planning and autonomic responses.
- Plays a role in empathy, social interaction, and predicting others’ behavior.
Clinical applications: Structural or functional changes in the cingulate gyrus are linked to OCD, depression, schizophrenia, and ADHD. Anterior cingulate dysfunction is often implicated in poor emotional regulation and reduced motivation.
Basal Ganglia (Limbic Region)
- Although often associated with movement, the limbic areas (especially the nucleus accumbens) are deeply involved in emotion, reward, and habit formation.
- Plays a central role in dopamine-based reinforcement learning, driving behaviors linked to pleasure and motivation.
- Connects emotional experiences to goal-directed behavior, helping form routines and habits.
Mental health link: Dysfunction in this region is implicated in addiction, compulsive behaviors, bipolar disorder, and Parkinson’s disease, where both movement and motivation are affected.
Interaction with Other Brain Regions
The limbic system does not function in isolation—it works in close partnership with other parts of the brain to shape our thoughts, emotions, and behaviors.
One key relationship is with the prefrontal cortex, which is involved in decision-making, impulse control, and social behavior.
This connection helps regulate emotional responses, allowing us to pause and think before reacting.
The brainstem also interacts with the limbic system, supporting automatic responses like heart rate and breathing during emotional arousal (e.g., fear).
These pathways explain why strong emotions can override logic and why emotionally charged memories are so vivid and long-lasting.
Treatment
Treatment approaches for limbic system-related difficulties are tailored to specific symptoms and underlying causes.
Mental health professionals may recommend psychotherapy to help manage emotional regulation challenges, anxiety, or depression stemming from limbic system dysfunction.
Cognitive behavioral therapy (CBT) can be particularly effective in addressing fear responses and emotional processing issues.
For severe cases, psychiatrists may prescribe medications like antidepressants or anti-anxiety drugs that help regulate limbic system activity. Some patients benefit from a combination of medication and therapy.
Self-care strategies can complement professional treatment:
- Maintaining regular sleep patterns to support limbic system function
- Practicing stress-reduction techniques like meditation or deep breathing
- Regular exercise to help regulate mood and reduce anxiety
- Establishing consistent daily routines to help with emotional regulation
- Avoiding known triggers that may overwhelm the system
Always consult healthcare providers to determine the most appropriate treatment plan, as needs vary significantly between individuals and conditions.
References
Banwinkler, M., Theis, H., Prange, S., & van Eimeren, T. (2022). Imaging the Limbic System in Parkinson’s Disease-A Review of Limbic Pathology and Clinical Symptoms. Brain Sciences, 12(9), 1248.
Bari, A., Niu, T., Langevin, J. P., & Fried, I. (2014). Limbic neuromodulation: implications for addiction, posttraumatic stress disorder, and memory. Neurosurgery Clinics of North America, 25 (1), 137–145.
Carmona, S., Vilarroya, O., Bielsa, A., Tremols, V., Soliva, J. C., Rovira, M., … & Bulbena, A. (2005). Global and regional gray matter reductions in ADHD: a voxel-based morphometric study. Neuroscience letters, 389(2), 88-93.
DelBello, M. P., Adler, C. M., & Strakowski, S. M. (2006). The neurophysiology of childhood and adolescent bipolar disorder. CNS Spectrums, 11 (4), 298-311.
Grèzes, J., Berthoz, S., & Passingham, R. E. (2006). Amygdala activation when one is the target of deceit: did he lie to you or to someone else?. Neuroimage, 30 (2), 601-608.
Gulyaeva, N. V. (2019). Functional neurochemistry of the ventral and dorsal hippocampus: Stress, depression, dementia and remote hippocampal damage. Neurochemical Research.
Herman, J. P., McKlveen, J. M., Ghosal, S., Kopp, B., Wulsin, A., Makinson, R., … & Myers, B. (2016). Regulation of the hypothalamic-pituitary-adrenocortical stress response. Comprehensive physiology, 6(2), 603.
Jhaveri, D. J., Tedoldi, A., Hunt, S., Sullivan, R., Watts, N. R., Power, J. M., … & Sah, P. (2018). Evidence for newly generated interneurons in the basolateral amygdala of adult mice. Molecular psychiatry, 23(3), 521-532.
Lepage, C., Muehlmann, M., Tripodis, Y., Hufschmidt, J., Stamm, J., Green, K., … & Koerte, I. K. (2019). Limbic system structure volumes and associated neurocognitive functioning in former NFL players. Brain Imaging and Behavior, 13 (3), 725-734.
Maletic, V., Robinson, M., Oakes, T., Iyengar, S., Ball, S. G., & Russell, J. (2007). Neurobiology of depression: an integrated view of key findings. International Journal of Clinical Practice, 61 (12), 2030-2040.
McEwen, B. S., Nasca, C., & Gray, J. D. (2016). Stress effects on neuronal structure: hippocampus, amygdala, and prefrontal cortex. Neuropsychopharmacology, 41(1), 3–23.
Morris, J. S., Frith, C. D., Perrett, D. I., Rowland, D., Young, A. W., Calder, A. J., & Dolan, R. J. (1996). A differential neural response in the human amygdala to fearful and happy facial expressions. Nature, 383 (6603), 812-815.
Okun, M. S., Bowers, D., Springer, U., Shapira, N. A., Malone, D., Rezai, A. R., Nuttin, B., Heilman, K. M., Morecraft, R. J., Rasmussen, S. A., Greenburg, B. D., Foote, K. D. & Goodman, W. K. (2004). What’s in a “smile?” Intra-operative observations of contralateral smiles induced by deep brain stimulation. Neurocase, 10 (4), 271-279.
Pagliaccio, D., Luby, J. L., Bogdan, R., Agrawal, A., Gaffrey, M. S., Belden, A. C., … & Barch, D. M. (2015). Amygdala functional connectivity, HPA axis genetic variation, and life stress in children and relations to anxiety and emotion regulation. Journal of abnormal psychology, 124(4), 817.
Piretti, L., Pappaianni, E., Lunardelli, A., Zorzenon, I., Ukmar, M., Pesavento, V., Rumiati, R. I., Job, R., & Grecucci, A. (2020). The role of amygdala in self-conscious emotions in a patient with acquired bilateral damage. Frontiers in Neuroscience, 14, 677.
Ponirakis, G., Ghandi, R., Ahmed, A., Gad, H., Petropoulos, I. N., Khan, A., … & Woodruff, P. W. (2022). Abnormal corneal nerve morphology and brain volume in patients with schizophrenia. Scientific Reports, 12(1), 1870.
Rolls, E.T. (2019). The cingulate cortex and limbic systems for emotion, action, and memory. Brain Structure and Function, 224(9), 3001-3018.
Sahin, N., Selouan, R., Markowitz, C. E., Melhem, E. R., & Bilello, M. (2016). Limbic pathway lesions in patients with multiple sclerosis. Acta Radiologica, 57 (3), 341-347.
Sergerie, K., Chochol, C., & Armony, J. L. (2008). The role of the amygdala in emotional processing: a quantitative meta-analysis of functional neuroimaging studies. Neuroscience & Biobehavioral Reviews, 32 (4), 811-830.
Stathis, P., Panourias, I. G., Themistocleous, M. S., & Sakas, D. E. (2007). Connections of the basal ganglia with the limbic system: implications for neuromodulation therapies of anxiety and affective disorders. Operative Neuromodulation, 575-586.
Tyng, C. M., Amin, H. U., Saad, M. N., & Malik, A. S. (2017). The influences of emotion on learning and memory. Frontiers in Psychology, 8, 1454.
Weissman, D. G., Lambert, H. K., Rodman, A. M., Peverill, M., Sheridan, M. A., & McLaughlin, K. A. (2020). Reduced hippocampal and amygdala volume as a mechanism underlying stress sensitization to depression following childhood trauma. Depression and anxiety, 37(9), 916-925.
White, T., Cullen, K., Rohrer, L. M., Karatekin, C., Luciana, M., Schmidt, M., Hongwanishkul, D., Kumra, S., Schulz, C. & Lim, K. O. (2008). Limbic structures and networks in children and adolescents with schizophrenia. Schizophrenia Bulletin, 34 (1), 18-29.
Xie, M., Yi, C., Luo, X., Xu, S., Yu, Z., Tang, Y., Zhu, W., Du, Y., Jia, L., Zhang, Q., Dong, Q., Zhu, W., Zhang, X., Bu, B., & Wang, W. (2011). Glial gap junctional communication involvement in hippocampal damage after middle cerebral artery occlusion. Annals of Neurology, 70(1), 121–132.
Yücel, M., Wood, S. J., Fornito, A., Riffkin, J., Velakoulis, D., & Pantelis, C. (2003). Anterior cingulate dysfunction: implications for psychiatric disorders?. Journal of Psychiatry and Neuroscience, 28 (5), 350.


